Objective: To review outcomes for men who undergo sacral neuromodulation (SNS) for refractory nonobstructive urinary retention or overactive bladder symptoms after prior surgery for benign prostatic hyperplasia (BPH).
Methods: We performed retrospective review of patients who had undergone a BPH procedure followed by a subsequent SNS procedure between January 2005 and March 2024. Clinical characteristics were collected, and outcomes were compared between different BPH procedure types as well as different indications for SNS using Chi-square, Fisher’s exact, and binomial logistic regression.
Results: We identified 24 men who had BPH surgery prior to subsequent SNS placement. As their indication for SNS, seven (29.2%) patients had persistent nonobstructive urinary retention (NOR) and 17 (70.8%) had overactive bladder (OAB) symptoms. Mean time between BPH and SNS procedure was 2.2 years. Ten patients (41.7%) experienced symptom relief with SNS with a mean follow up duration of 34.0 months.
Conclusion: Men with refractory NOR or OAB after prior BPH surgery rarely undergo SNS. In men who do undergo SNS, overall success rates are low, and age, time between procedures, indication, and type of prior BPH surgery do not appear to predict rates of success with SNS.
Keywords: Benign prostatic hyperplasia, Overactive bladder, Nonobstructive urinary retention, Sacral neuromodulation, Sacral nerve stimulator
Benign prostatic hyperplasia (BPH) is one of the most common conditions affecting aging males and is the leading cause of lower urinary tract symptoms (LUTS). Treatment of BPH focuses on addressing obstructive and/or irritative voiding symptoms that result from prolonged bladder outlet obstruction. Upwards of 30% of men have overactive bladder (OAB) symptoms concurrently with obstructive symptoms characteristic of benign prostatic obstruction.1 There are several surgical options including, but not limited to, prostatic urethral lift (UroLift), prostatic water vaporization (Rezum), transurethral resection of prostate (TURP), photovaporization of prostate (PVP), holmium laser enucleation of prostate (HoLEP), and simple prostatectomy.2
While these interventions are generally very effective, 30-40% of men report persistent or de novo irritative voiding symptoms characterized by urgency, frequency, and incontinence in the early post-operative period.3 Although many patients have improvement in symptoms by 3 months, several others may have persistent symptoms requiring additional therapeutic management.4,5 On the other hand, a handful of men with preoperative urinary retention continue to have nonobstructive urinary retention (NOR) despite treatment of their BPH due to bladder de-functionalization from long-standing outlet obstruction.6
Sacral neuromodulation (SNS) is a minimally invasive procedure that is currently approved and offered as third-line treatment for patients with OAB, or those with non-obstructive urinary retention (NOR).7,8 Long-term efficacy and safety of SNS in women is well-established, with therapeutic response rates reported ranging from 60-80%.9 Outcomes for men are less well described, as most studies have a majority of female patients and contain a minority of male subjects.10 There is a dearth of literature on the efficacy of SNS for OAB and NOR in the male population and particularly for men who have refractory urinary symptoms despite surgical treatment of their BPH. We sought to expand on the literature by reflecting on our institutional experience and outcomes for men who undergo SNS for persistent urinary symptoms after BPH surgery.
Under institutional review board (IRB) approval, we conducted a review of our institution’s electronic database warehouse (EDW) for men over 18 who had undergone a BPH procedure and an SNS procedure from January 2005 to March 2024. CPT codes were used to identify procedure events and the BPH procedures queried included prostatic urethral lift (UroLift), prostatic water vaporization (Rezum), transurethral resection of prostate (TURP), greenlight photovaporization of prostate (PVP), holmium laser enucleation of prostate (HoLEP), and simple prostatectomy. Similarly, CPT codes were used to identify SNS events. Peripheral tibial nerve stimulation (PTNS) was not included in our search. We then excluded patients who had SNS performed prior to BPH surgery to obtain our final cohort of men who underwent SNS after their BPH procedure.
Manual retrospective chart review was performed to collect baseline characteristics and outcomes data. Baseline characteristics collected included age, BMI, procedure dates, procedure type, catheter dependence, preoperative International Prostate Symptom Score (IPSS), preoperative post void residuals (PVR), and use of BPH or OAB medications, if available. BPH medications include alpha-blockers and 5-alpha-reductase inhibitors. OAB medications include anticholinergics and adrenergic beta-3 receptor agonists. Other data collected included postoperative IPSS, postoperative PVR, whether patients had urodynamic studies (UDS) performed prior to SNS placement, and any use of intravesical botulinum toxin prior to SNS. Primary outcomes of interest included time elapsed between BPH and SNS procedures, reason for undergoing SNS placement, whether SNS was successful in symptom relief, follow up duration, and whether SNS was explanted if ineffective. Determination of success was based on provider documentation of patient symptom improvement in the electronic medical record (EMR).
All data analyses were performed using SPSS (IBM SPSS Statistics for Windows v.29). Descriptive statistics and comparisons between groups were performed with Chi-square and Fisher’s exact test when appropriate. Binomial logistic regression was used to determine if clinical characteristics were associated with successful symptom relief with SNS. ANOVA was used to compare means between BPH procedure groups. For all analyses, a cutoff of p<0.05 was considered statistically significant.
We identified 31 men between January 2005 and March 2024 who had undergone both a BPH procedure and a SNS procedure within the institution’s healthcare system. We then reviewed procedure dates and excluded men who had undergone SNS prior to BPH surgery to limit our cohort to patients who underwent BPH surgery first. A total of 24 men were identified and included in the final analysis. As their index BPH procedure, 3 (12.5%) patients received UroLift, 1 (4.2%) Rezum, 10 (41.7%) TURP, 8 (33.3%) PVP, and 2 (8.3%) HoLEP. There were no patients in our cohort that underwent simple prostatectomy as their index BPH procedure.
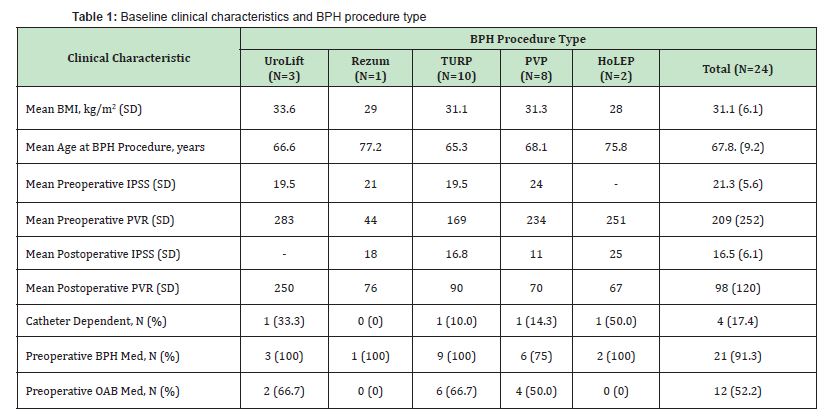
Table 1 shows clinical characteristics for the overall cohort, as well as for each type of BPH procedure. Overall, mean age at initial BPH procedure was 67.8 years, mean BMI was 31.1, mean preoperative IPSS was 21.3, and mean preoperative PVR was 209mL. Mean postoperative IPSS after BPH was 16.5 and mean postoperative PVR was 98mL after initial BPH procedure. Four patients (17.4%) were catheter dependent preoperatively, twenty-one (91.3%) were taking a BPH medication, and twelve (52.2%) were taking medication for OAB symptoms. On subgroup analysis, there were no statistically significant differences amongst different BPH procedure groups in any of these clinical characteristics (p>0.05).
As shown in Table 2, the mean time between index BPH procedure and subsequent placement of SNS was 2.2 years. Nonobstructive urinary retention (NOR) was the indication for SNS placement in 7 (29.2%) men while overactive bladder (OAB) was the indication in 17 (70.8%) men. Fourteen men (58.3%) had urodynamic (UDS) testing prior to their SNS procedure. There was no significant difference in rates of UDS testing between NOR and OAB groups. Four (57.1%) of the 7 men with NOR and 10 (58.8%) of the 17 men with OAB had UDS. UDS testing was not associated with increased rates of success with SNS (43% vs 40%, p>0.05). Fifteen patients (62.5%) were taking medication for OAB symptoms and eight (33.3%) had trialed intravesical botulinum toxin therapy for their symptoms prior to SNS. Overall, SNS was successful in improving symptoms in 10 patients (41.7%) with a mean follow up duration of 34.0 months. Six patients (25%) ultimately had their SNS explanted due to poor efficacy.
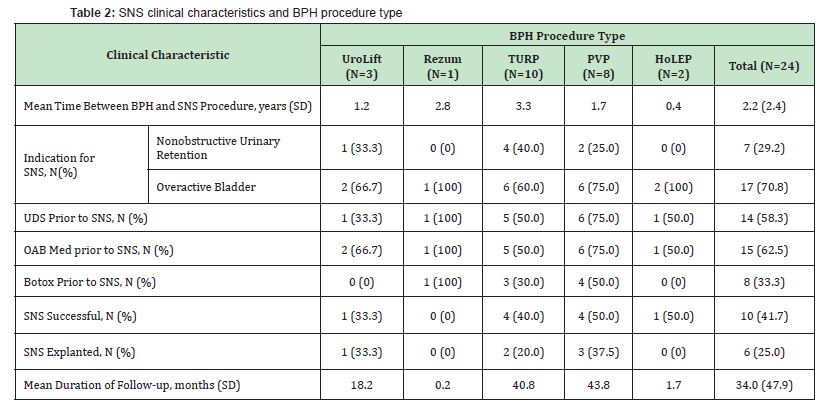
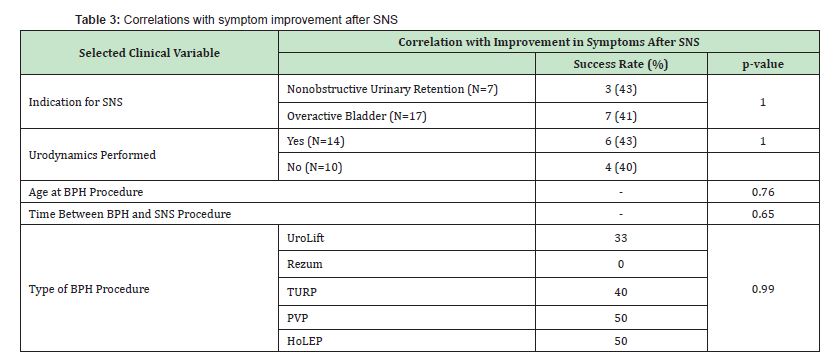
Table 3 shows the correlations between successful symptom relief with SNS and selected clinical variables. Success rate of SNS was not significantly different based on indication for SNS, with 3 (43%) patients having symptomatic improvement of nonobstructive urinary retention and 7 (41%) patients having improvement in overactive bladder symptoms (p=1.00). Furthermore, age at BPH procedure (p=0.76), time interval between BPH and SNS procedures (p=0.65), and type of BPH procedure (p=0.99) were not correlated with increased rates of effectiveness.
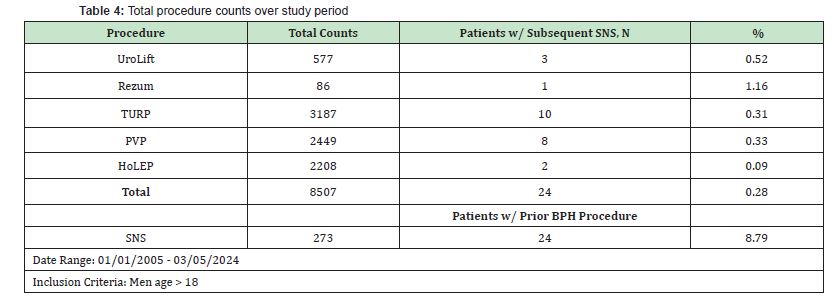
Between January 2005 and March 2024, there was a total of 577 UroLift, 86 Rezum, 3187 TURP, 2449 PVP, and 2208 HoLEP procedures performed. The percentage of patients that had subsequent SNS after BPH surgery is reflected in Table 4. Apart from the Rezum group, which only had one patient, rates were under 1%, with an overall rate of 0.28%. There was also a total of 273 SNS procedures performed. Twenty-four out of 273 patients (8.79%) who underwent SNS had prior BPH surgery. Six (25%) patients had history of multiple BPH procedures. One patient had UroLift followed by TURP prior to SNS, and two patients had multiple TURPs prior to SNS. Three patients had TURP followed by SNS, and subsequently underwent repeat TURP or PVP after failure of SNS to improve urinary symptoms.
Sacral neuromodulation (SNS) is a guideline-directed, well-established third line therapy for refractory overactive bladder symptoms and nonobstructive urinary retention.7 Although the exact mechanism of SNS has not yet been elucidated, it is postulated that the therapy alters spinal cord reflexes by modulating afferent input into the sacral spinal cord, which in turn may help modulate detrusor over and under-activity.11,12 The overall efficacy of SNS in urinary symptom improvement is high, with patient satisfaction ranging from 60% to as high as 85% in some studies.13,14 The majority of patients undergo SNS for overactive bladder symptoms, but its efficacy for management of nonobstructive urinary retention appears to be similar.6,15 However, SNS has traditionally been studied in women, and the efficacy in men is not as well understood mainly due to underuse in this patient population.16-18 We sought to reflect on our experience and outcomes for men who undergo SNS placement for refractory nonobstructive urinary retention or overactive bladder symptoms after prior BPH surgery.
In our institutional experience, men rarely progress to needing SNS after BPH surgery and rates of SNS placement in men overall appear to be low. Between January 2005 and March 2024, there were 8507 total documented BPH surgeries performed and only 24 (0.28%) patients had subsequent SNS placement. Only 273 men in total underwent SNS placement over the period in our hospital system. Of these 273 patients, fewer than 10% had undergone a prior BPH surgery. These findings suggest two conclusions- BPH procedures are highly effective in relieving most urinary symptoms for men, and providers seem to be able to distinguish men who would benefit from initial SNS placement rather than a bladder outlet procedure. In comparison, over the same time-period from January 2005 to March 2024, there were 1418 SNS procedures performed in women. Prior studies have shown that men may have similar rates of satisfaction with SNS as women.18 More work in this space is needed to determine if more men may be able to benefit from SNS, as it currently appears to be an underutilized therapy in men.
In men with refractory urinary symptoms after BPH surgery who did progress to sacral neuromodulation, we did not see any statistically significant differences in age, BMI or preoperative clinical characteristics such as preoperative IPSS or post void residuals between the different BPH surgery groups. The mean time between index BPH procedure and subsequent SNS placement was 2.2 years. This number appears reasonable as there is an established post-BPH surgery recovery period where patients may experience transient worsening of their irritative voiding symptoms for the first 3 months up to 1 year.17 Occasionally, a handful of men may have persistent voiding issues that require secondary therapy such as intravesical botulinum toxin A (botox) injection. In our cohort, 15 patients (63%) were taking medication for overactive bladder symptoms and 8 patients had a trial of intravesical botox prior to SNS.
Urodynamics (UDS) allows clinicians to assess abnormalities in urinary storage and voiding such as bladder capacity, compliance, pressures, and detrusor hypo- and hyper-activity. Results of urodynamic testing help guide decision making and selection of appropriate therapy for patients. In our cohort, UDS was performed in 14 (58.3%) of 24 men prior to SNS, with a relatively equal distribution between men with NOR and OAB (57.1% vs 58.8%). Of the 4 patients with NOR who underwent UDS, UDS confirmed inability to generate detrusor contraction in 3. Of the 10 patients with OAB who underwent UDS, only 4 had hypersensitivity or detrusor overactivity (DO) seen on the study. There was no association between UDS result and SNS success in our limited cohort. Interestingly, of the 3 patients with NOR who experienced symptom relief with SNS, all had UDS performed. In comparison, out of the 7 patients with OAB who had symptomatic improvement with SNS, only 3 had UDS. While this may suggest more accuracy or utility of UDS in men with NOR compared to OAB, ultimately our sample sizes were too small to see statistical significance and too small to draw any meaningful conclusions.
Sacral neuromodulation was successful in 10 (41.7%) of 24 patients in improving urinary symptoms at a mean follow-up of 34 months. While the efficacy rate appears to be lower than the 70-80% described in prior literature, the men in our cohort likely represent a patient population that is more difficult to treat. Men in our cohort have failed pharmacologic therapy as well as surgical therapy for BPH suggesting potentially more severe baseline pathology causing their urinary symptoms. Prior studies include BPH-treatment naïve patients or do not specify prior history of bladder outlet surgeries. While our reported success rates here are moderate, there was no difference in success rates between men with refractory nonobstructive urinary retention (NOR) and those with persistent overactive bladder symptoms (OAB). Three out of 7 NOR patients (43%) and seven out of 17 (41%) OAB patients reported symptom improvement. In women, reported rates of success are similar between nonobstructive urinary retention and overactive bladder.14,15 In our cohort, it appears that SNS has similar moderate efficacy and durability in men with indication. Ultimately, six men (25%) had their SNS explanted due to ineffectiveness. None were explanted due to infection. A systematic review by Ho et al found that the explantation and/or revision rate is usually less than 20%.6 Typical reasons for explantation or revision include ineffective device, device migration, infection, incorrect initial placement, and need for MRI compatibility. Newer sacral neuromodulation devices are now MRI compatible and rarely explanted for this reason alone. Slightly higher explantation rate in our cohort is likely reflective of the lower rates of success in our patient population.
It remains unclear whether there are clinical characteristics that may help providers predict which patients may ultimately fail pharmacologic and surgical BPH treatment for their urinary symptoms and progress to SNS. This is outside the scope of this study as we did not compare our cohort to patients who underwent BPH surgery who did not undergo SNS, however it remains an important future question of interest. We did seek to determine if there were any clinical factors that predicted success with SNS placement. A prior study by Noblett, et al. demonstrated that patients with more severe baseline symptoms had statistically similar success rates and symptomatic improvement to patients with less severe symptoms with regards to both urinary frequency and urinary incontinence episodes.19 In our study we found that age, preoperative IPSS, preoperative PVR, and preoperative medication use were not significantly associated with change in rates of success. Time between BPH and SNS procedures as well as specific type of BPH procedure was also not correlated with different rates of success. Unfortunately, our ability to determine true preoperative symptom quality and severity in our cohort is limited to some degree due to its retrospective nature and incompleteness of the electronic medical record (EMR) and documentation going back over the past twenty years. Similarly, success was determined through reviewing provider documentation in the EMR, however there were no consistent objective measures used by each provider to dichotomize success and failure.
There are several limitations to this study, namely its retrospective nature and small sample sizes due to the low incidence of events. Sacral neuromodulation was developed in 1982 by Tanagho and Schmidt and was approved by the Food and Drug Administration (FDA) for use in treating urinary incontinence in the U.S. since 1997.20 In 1999, SNS was approved for urinary retention and urinary frequency symptoms. We tried to cast a wide net and capture all events in our hospital system over the past twenty years to gain insight to the landscape of how SNS is being used in men, particularly those with prior failed BPH intervention. Even so, our data likely underestimates the true incidence of men progressing to SNS after prior BPH surgery, as our data only includes men who have had both procedures performed within our system. We were not able to capture men who had a BPH procedure in our system and perhaps moved on to have SNS placement elsewhere. Similarly, we were not able to capture men who had an SNS placed in our system who had prior BPH surgery elsewhere. Thus, the true incidence is likely higher than what we report here.
As mentioned previously, due to the retrospective nature and incompleteness of the EMR, it was difficult to assess the true impact of SNS placement for each patient. The definition of success used in this study was solely based on provider documentation of reported improvement in patient symptoms rather than concrete criteria such as greater than 50% reduction in pad use, leakage episodes, or urinary frequency. Objective measures such as PVRs, uroflow, or urodynamic studies were also not routinely completed or documented postoperatively to allow for comparison. Similarly, validated surveys were not completed for all patients. All patients had reported symptomatic improvement with percutaneous SNS lead placement in their trial period prior to proceeding with second stage implantation. Our data suggests that SNS is moderately efficacious for patients with refractory NOR or persistent OAB after BPH surgery, however additional studies will be needed to determine its efficacy in a prospective, standardized manner.
In our experience, men with refractory nonobstructive urinary retention or overactive bladder symptoms after prior BPH surgery rarely progress to needing sacral neuromodulation. Men with refractory NOR or persistent OAB have moderate rates of symptom improvement suggesting that SNS may be underutilized in this space. In those who do undergo subsequent sacral neuromodulation, age, time between procedures, indication, and type of prior BPH surgery do not appear to predict rates of success with SNS.
This study was approved by the Northwestern University Institutional Review Board under study number STU00220137.
Not applicable.
This Research Article received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Dr. Amy Krambeck is a consultant for Boston Scientific, Wolf, Storz, and Virtuoso Surgical. She is a data safety monitoring board member of Sonomotion and Uriprene. The other authors have no conflict of interests or disclosures.

