First described by Barlow and Dickson in 1978, the purple urine bag syndrome (PUBS) is an infrequent condition that even if it ́s benign, it seems to be alarmant. It consists on the purple coloring of the urine inside the colector bag, which is the result of a chemical reaction between the enzymes that produce phosphate and sulfates, the patient’s diet and the intestinal transit.
Keywords: Urine, Urinary Catheterization, Urinary Tract Infections, Prostration, Antibiotic
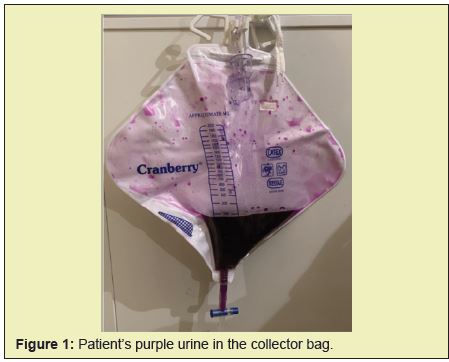
A 78-year-old man with a history of prostration due to advanced Parkinson's disease, user of an indwelling urinary catheter (IDC) due to benign prostatic hyperplasia, admitted to the emergency department for five days of qualitative-quantitative compromise of consciousness and un quantified fever. The reason for the consultation was dysfunctional IDC, with lack of urinary output of 24 hours of evolution. On febrile admission sinus tachycardia of 101bpm, normotensive. A bedside echoscope was performed, which confirmed the bladder balloon. The catheter was changed, giving cloudy urine which turned purple in the collection bag (Figure 1). The urinalysis revealed a pH of 8.0 [N.V. 4.5-8.0] positive nitrites and leukocyturia> 100 per field. Urine culture was positive> 100,000u.f.c. for Klebsiella pneumonia sensitive to ceftriaxone. After 48 hours of antibiotic treatment, the urine turned a normal color. The patient completed antibiotic treatment and was discharged.
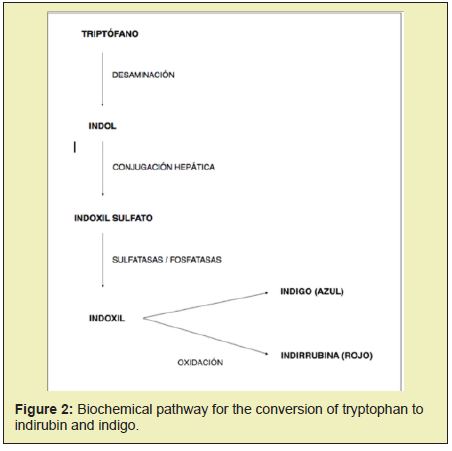
Purple urine bag syndrome occurs more frequently in elderly people, mainly women. IDC users or long-term users, patients with chronic kidney failure, bedridden or with reduced mobility and chronic constipation.1,2 Indole is produced by the bacterial degradation of tryptophan provided in the diet by bacteria of the intestinal flora. Once absorbed via the portal, it is transformed in the liver to indoxyl sulfate, which is excreted in the urine. In the presence of the bacterial enzyme indoxyl-sulfatase, indoxyl sulfate is hydrolyzed to indoxyl, which in an alkaline environment - favored by the presence of sulphatase and phosphatase-producing bacteria that also present the enzyme urease, which alkalizes urine- generates indirubinpigments. (Red color) and (Indigo blue color). These in turn precipitate by reacting with the polyvinyl chloride from which the probes and collection bags are made, forming a red, blue or purple coating layer. (Figure 2)The main bacteria involved in this phenomenon are Escherichia coli, Klebsiella pneumonia, Pseudomonad aeruginosa, Morganella morganii, Proteus mirabilis y vulgaris, Enterococcus agglomerans, avium, facials, cloacae, Providencia stuardii y rettgeri, Citrobacter koseri, freundiiydi versus.3,4 The exact prevalence of PUBS is unknown. The vast majority of the publications are reports of clinical cases, and there are no studies with significant sample sizes. A prevalence of 9.8% is estimated in patients with an indwelling urinary catheter.5,6 There are no data about its prevalence in Chile.4 Purple urine bag syndrome is a benign entity, urine normally returns to its normal color when bacteriuria resolves and urine becomes acidic. Among the differential diagnoses, the intake of substances that change the color of the urine should be considered, such as methylene blue, iodinated compounds, beets, amitriptyline, indomethacin, and cyanocobalamin. And pathologies such as porphyria, Drummond syndrome (familial hypocalcaemia with nephrocalcinosis. 4,7,8
None.
None.
Author declares that there is no conflict of interest.
- 1. Harun NS, Nainar SK, Chong VH. Purple urine bag syndrome: a rare and interesting phenomenon. South Med J. 2007;100(10):1048–1050.
- 2. L. Fernández de Orueta, J. EstebanFernández, G. Pérez Caballero, et al. Brief Papers About Basic Research Or Clinical Experiences. Nefrologia. 2011;31(4):489–504.
- 3. Dealler SF, Hawkey PM, Millar MR. Enzymatic degradation of urinaryindoxyl sulfate by Providen ciastuartii and Klebsiella pneumoniae causes the purple urine bag syndrome. J Clin Microbiol. 1988; 26(10):2152–2156.
- 4. Chassin-Trubert, A. Síndrome de la bolsa de orina púrpura: un fenómeno inusual y muy llamativo. Rev Med Chile. 2014;142:1482–1484.
- 5. Hadano Y, Shimizu T, Takada S, et al. An update on purple urine bag syndrome. Int J Gen Med. 2012;5(1):707–710.
- 6. Dealler SF, Belfield PW, Bedford M, Whitley AJ, Mulley GP. Purple urine bags. J Urol. 1989;142(3): 769–770.
- 7. Tan CK, Wu YP, Wu HY, Lai CC. Purple urine bag syndrome. Can Med Assoc J. 2008;179(5):491.
- 8. Raymond JR, Yarger WE. Abnormal urine color: Differential diagnosis. South Med J. 1988;81(7): 837–841.

