Background: Chronic kidney disease is a non-communicable global problem. In patients of chronic kidney disease especially in Hemodialysis patient mortality and morbidity due to atherosclerosis induced cardiovascular complications is very high despite the advances of Hemodialysis procedure. Residual renal function contributes significantly to the overall health and cardiovascular morbidity of dialysis patients. So, the loss of residual renal function, especially in patients on Hemodialysis, is a powerful predictor of mortality. Preserving residual renal function is the goal of nephrologists.
Objective: To find the association between residual renal function and cardiovascular morbidity in twice weekly and thrice weekly Hemodialysis patient.
Methodology: This cross sectional study was conducted on 72 Hemodialysis patients received dialysis more than three months in the dialysis centre of BSMMU and DMCH, Dhaka, Bangladesh during the period of October 2018 to September 2019. Study populations were divided into two groups on the basis of residual renal function (RRF). RRF was defined by interdialytic 24 hours urine volume and average of urinary urea and creatinine clearance. Preserved RRF was defined 24 hours urine volume more than 100ml. Chi-square test (χ2), Student’s paired t-test and multiple regression analysis were used to find association between cardiovascular morbidity and RRF.
Result: A significant difference of diastolic dysfunction, systolic dysfunction, LVH (p=0.001, p=0.001, p=0.004 respectively) was seen in between preserved RRF and without preserved RRF group but the difference of regional wall motion abnormality and valvular heart disease was found to be non-significant. In regression analysis, loss of RRF was found to be a significant predictor of cardiovascular morbidity
Conclusion: Preserved RRF was significantly associated with less frequent diastolic dysfunction, left ventricular hypertrophy and higher level of left ventricular ejection fraction compared to without preserved residual renal function in both twice weekly and thrice weekly HD patient.
Keywords: Chronic Kidney Disease (CKD), Hemodialysis, Residual Renal Function (RRF), Morbidity, Dysfunction, Abnormality, Nephrologists
Chronic kidney disease (CKD) is a global public health problem. As the number of diabetic patients is increasing, CKD patients is also increasing and with nearly 30% of the 170 million diabetic patients eventually developing diabetic Nephropathy.1 Arge proportion of patient with chronic kidney disease eventually develop end stage renal disease (ESRD) with the need for dialysis or kidney transplantation. ESRD incidence increased by 94% from 1990 to 2015.In 2015, 124,114 patients initiated treatment for ESRD, 120,972 of whom started on dialysis (3,142 start with a kidney transplant).Worldwide, most patients with end-stage renal disease (ESRD) start treatment with Dialysis and only ~2% get access to renal transplantation.2 The end stage renal disease (ESRD) patients have been increasing in Asian countries also but every country has its own barriers to provide better dialysis which has the same standard like developed countries.3 With time being, the advances in HD procedure, mortality remains high in patients undergoing HD compared with the general population due to accelerated atherosclerosis, resulting in a higher risk of cardiovascular death.4 Sudden death, myocardial infarction, cardiac arrest, malignant arrhythmias and other cardiac causes is the major cause of death accounting for 43% of all-cause mortality among Hemodialysis patients. Not only traditional risk factors, Hemodialysis patients but also have a number of nontraditional cardiovascular risk factors including persistent low-grade inflammation, metabolic acidosis, volume overload, and co morbidities, which play a prominent role in the development of Left ventricular hypertrophy, coronary artery disease, rapid electrolyte shifts, QT dispersion, sympathetic over activity, calcium-phosphate deposition.5,6
Residual renal function (RRF) is in general defined as the residual glomerular filtration rate (rGFR) in patients with ESRD. (B Marron, ISN) Residual renal function (RRF) may provide many ben¬efits that are related to better volume control and greater solute clearance, playing a crucial role in the achievement of a sufficient dialysis treatment.7,8 Moreover, RRF is accompanied by more phosphate urinary ex¬cretion, better control of secondary hyperparathyroidism, improved nutritional markers, better endogenous vi¬tamin D and erythropoietin production removal of middle molecular uremic toxins, and shows strong inverse relationships with valvular calcification and cardiac hypertrophy in dialysis patients.9‒13 Therefore less cardiovascular morbidity and mortality. So longer preservation of RRF is the goal in HD In developed countries, a dialysis frequency of 3 times per week is the current standard practice to achieve an adequate dialysis dose, and the Kidney Disease Outcomes Quality Initiative (KDOQI) guideline recommends thrice-weekly treatment in patients without RRF. However, a reduction in the frequency of dialysis can be considered in patients with substantial RRF.10 Indeed, there are some reports that twice-weekly dialysis does not increase mortality risk in comparison with thrice-weekly therapy, and it is suggested that a twice-weekly regimen is a valid option in cases of HD patients with RRF.11,12 Therefore, RRF preservation contributes considerably to the im¬provement of quality of life, cardiovascular protection, and even better survival in this patient population.13
This cross sectional study was carried out in the department of Nephrology, Bangabandhu Sheikh Mujib Medical University (BSMMU), Dhaka, Bangladesh and department of Nephrology, Dhaka Medical College & Hospital (DMCH), Dhaka, Bangladesh from October 2018 to September 2019. According to the statistical calculation a total of seventy two (72) CKD patients on MHD were enrolled in this study by convenient purposive sampling following selection criteria. Patients of end stage renal disease (ESRD) on maintenance Hemodialysis (MHD) for at least 3 months, age 18 to 70 years of both sexes were included in this study. Renal transplant recipients resuming dialysis due to graft dysfunction, patients on shift of dialysis, patients having inter-dialytic weight gain more than 5% of total body weight, patients had calculated stdKt/V urea less than 1.45 in twice weekly and less than 2 in thrice weekly Hemodialysis and patients with known case of coronary artery disease before beginning of Hemodialysis were excluded from this study. All participants were explained about the objectives, nature, purpose and potential risk of all procedures used for the study prior to enrollment. On the basis of patient record file, interview of the patient, dialysis staffs and patient caregiver sample were recorded into twice and thrice weekly Hemodialysis. Blood samples were taken before and immediately after dialysis to determine KT/V urea/session and to see the electrolytes, calcium and phosphate level& lipid profile. Sp KT/V was calculated from Daugirdas formula. Sp KT/V was calculated in every dialysis of a week in each sample to measure std KT/V urea. Blood pressure was measured at the beginning and thereafter 2 hours of HD following standard procedure.
Residual renal function was measured in all patients treated with dialysis by determining the glomerular filtration rate as the arithmetic mean of the urinary clearances of urea and creatinine clearance. Clearance was calculated from urea and creatinine concentrations in urine collected during the 24 hours before the first Hemodialysis session of the week. All the biochemical parameters of blood and urine were estimated by Germany made Photometer 5010 V5+ analyzer. Those who had urine volume more than 100ml was taken as preserved residual renal function (RRF) and those with less than 100ml urine. According to RRF preservation, the study group was divided into preserved RRF (Group-A) and without preserved RRF (Group-B). Two dimensional and M-mode echocardiogram was performed using a M2540A model Philips echocardiograph by cardiologist to evaluate the patients for regional wall motion abnormality, wall thickness and chamber dimensions, ejection fraction and diastolic dysfunction. Computer based statistical analysis was carried out with appropriate techniques and systems. All data were recorded systematically in preformed data collection form. Quantitative data were expressed as mean and standard deviation and qualitative data were expressed as frequency distribution and percentage. Statistical analyses were performed by using windows based computer software with Statistical Packages for Social Sciences (SPSS-22) (SPSS Inc, Chicago, IL, USA). Association between categorical variables was done by chi-square test and continuous variable by t-test. Multiple regression analysis was done to see any relationship between RRF and cardiovascular morbidity. For all statistical tests, p value <0.05 was considered as statistically significant.
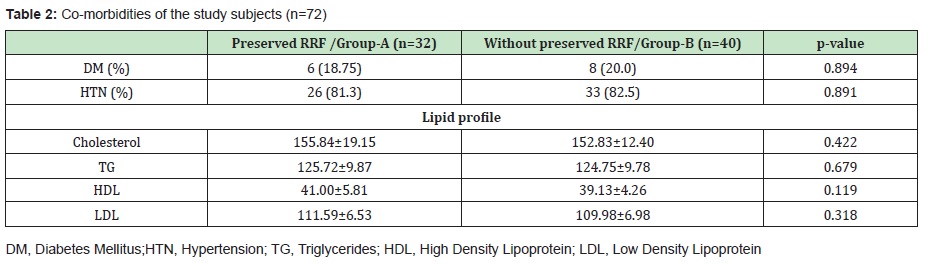
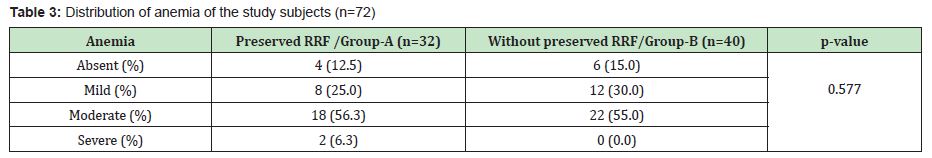
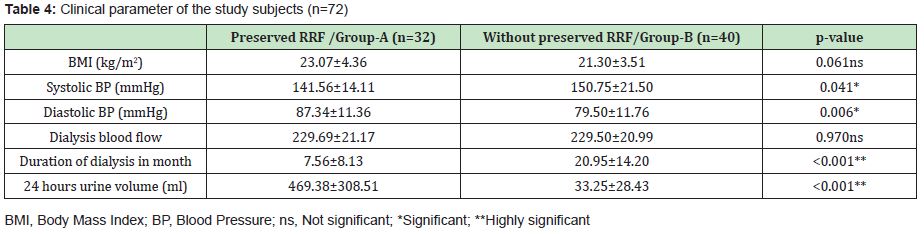
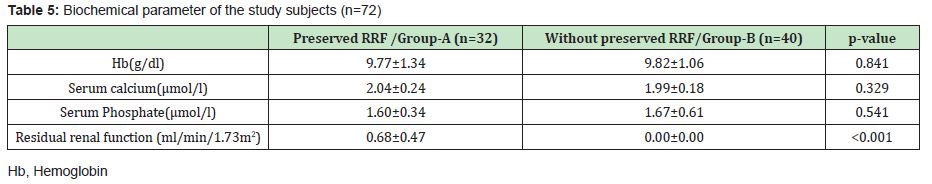
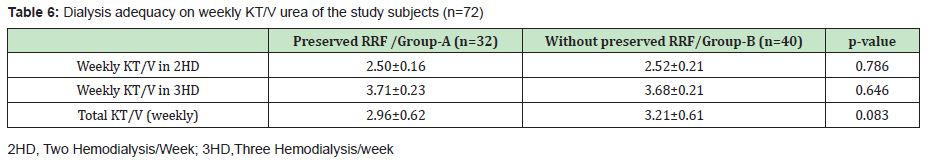
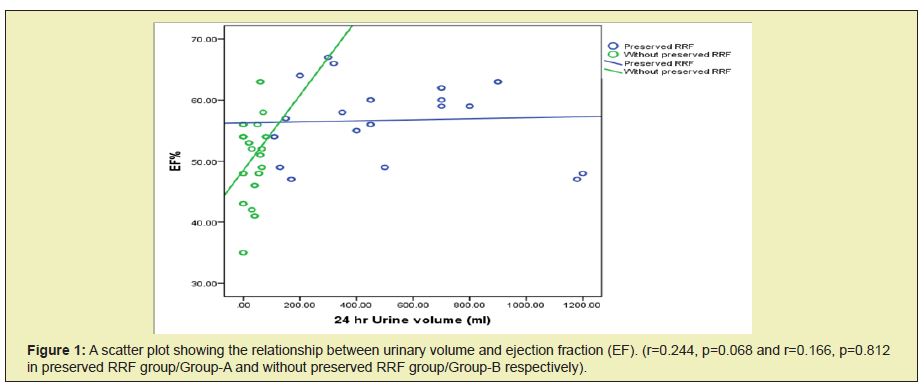
A total of 72 CKD patients on MHD were evaluated to find association between residual renal function (RRF) and cardiovascular morbidity. Among them 32 (44.44%) were in Group-A (Preserved RRF) and 40 (55.55%) were in Group-B (Without preserved RRF). Mean±SD age of the study patients was 43.22±16.93 years and 41.95±15.35 years in Group-A and Group–B respectively. Among total study patients 46 (63.88%) were male and 26 (36.11%) were female, of them 22 (68.8%) male and 10 (31.3%) female were in Group-A while 24 (60%) male and 16 (40%) female were in Group-B. Among 32 Group-A patients 20 (62.5%) were taking twice weekly hemodialysis (2HD/week) and 12 (37.5%) were taking thrice weekly hemodialysis (3HD/week). It was observed that most of the patients in two groups were male and the age difference between the groups was not statistically significant (p=0.740). Majority of the patients in Group-A were taking twice weekly HD, but in Group-B thrice weekly HD was more, although the differences were not statistically significant (p=.0.048 in 2HD/week and p=0.060 in 3HD/week) (Table 1) Values in the parenthesis denote corresponding percentage Values in the parenthesis denote corresponding percentage Table 2 shows that there was similar frequency of DM, HTN and lipid abnormalities between two groups. It was observed that subjects with preserved RRF (Group-A) and without preserved RRF (Group-B) had similar level of anemia. Moderate anemia was more pronounced in both groups (Table 3). Values in the parenthesis denote corresponding percentage. There were no significant differences in BMI and dialysis blood flow among the patients of Group-A and Group-B (p=0.061 and p=0.970 respectively). While diastolic blood pressure and 24 hours urine volume were significantly (p=0.006 and p<0.001)) lower in Group-B but Systolic blood pressure (p=0.041) was significantly higher in Group-B (Table 4). Table 5 shows that patients of both Group-A and Group-B had almost similar serum calcium, serum phosphate and hemoglobin level. Residual renal function was significantly higher in Group-A (p<0.001). There was similar dialysis adequacy in Group-A and Group-B on the basis of dialysis schedule (Table 6). It was observed that there was significant higher level of left ventricular hypertrophy (LVH), systolic dysfunction and diastolic dysfunction in Group-B than Group-A. There were no significant differences in wall motion abnormality and valvular heart diseases among patients of both groups. While ejection fraction (EF) of the patients in Group-A was significantly higher than patients in Group-B (Table 7). Values in the parenthesis denote corresponding percentage multiple logistic regression analysis shows that age, dialysis duration and residual renal function (RRF) were independently associated with cardiovascular morbidity. RRF correlates 7.5 times with cardiovascular morbidity. No significant co-relation was observed between cardiovascular morbidity with BMI, age, DM, HTN and lipid profile (Table 8). The relationship between urinary volume (ml) and ejection fraction (%) is displaying in Figure 1.
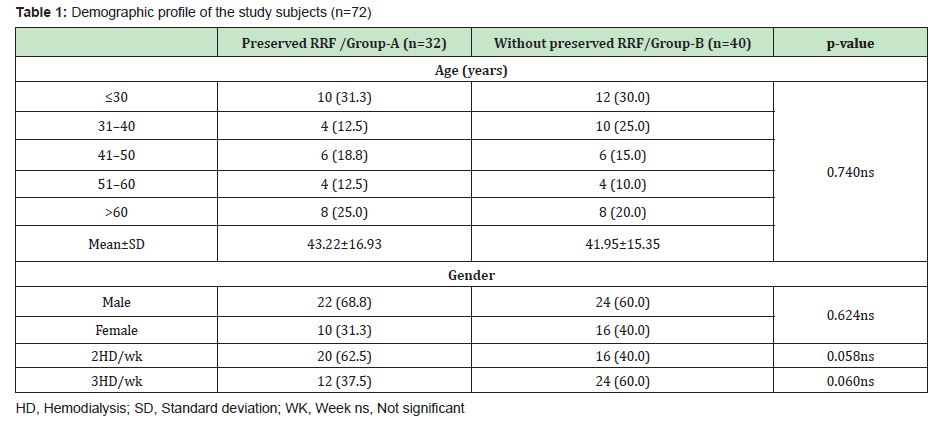
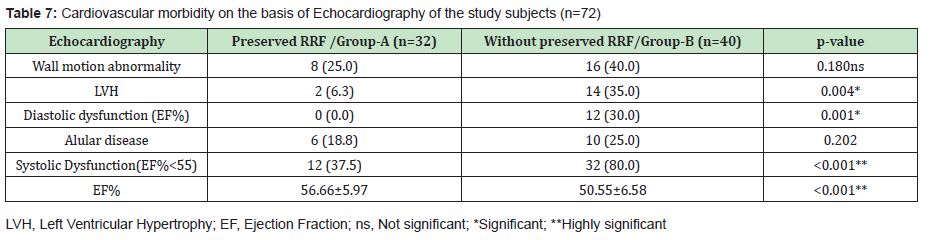

To our knowledge, this was the first cross sectional study in Bangladesh to see the association of RRF with cardiovascular morbidity in dialysis patients. It was observed that there was significant higher number of left ventricular hypertrophy (LVH), systolic dysfunction and diastolic dysfunction in Group-B than Group-A. There were no significant differences in wall motion abnormality and valvular heart diseases among patients of both groups. While ejection fraction (EF) of the patients in Group-A was significantly higher than patients in Group-B. In a study conducted by Raikou VD showed the similar significant higher level of diastolic dysfunction, LVH but non-significant higher level of systolic dysfunction between without preserved RRF and preserved RRFgroup.14‒17 Mean age was similar in the two group (43.22±16.93 vs 41.95±15.35, p=0.74). Highest of patients were in age group <30 years and ˃60 years. Males were predominant in both groups. There was no significant age and gender difference between these two groups.18‒21 Similar age and gender distribution was observed in a study by Mukherjee T et al.22 This may be explained by the observation that ESRD are more prevalent in this group. Mean age of the patient was also higher in the study by Hwang HS et al. comparing this study.16
Hypertension was most common co-morbid condition of the two groups (preserved RRF group and without preserved RRF group was 81.3% versus 82.5% respectively). There was no statistically significant difference of lipid profile among the patients in both groups. LDL-Cholesterol was most abnormal lipid in both groups. There were no significant differences in BMI and dialysis blood flow among the patients of Group-A and Group-B (p=0.061 and p=0.970 respectively). While diastolic blood pressure and 24 hours urine volume were significantly (p=0.006 and p<0.001)) lower in Group-B but Systolic blood pressure (p=0.041) was significantly higher in Group-B. Therefore it was observed that in preserved RRF group had significant higher level of 24 hours urinary volume (469±308 vs 33±28, p=0.002) than without preserved RRF group. Both the preserved and without preserved RRF group had twice weekly and thrice weekly HD patient. Thrice weekly HD reduced the RRF early. In a study done by Saeed et al. also showed the decline in residual kidney function was slower in patients dialysing twice versus thrice weekly.19 In this study the frequency of twice weekly HD and thrice weekly HD in both the group was statistically non-significant. Urinary excretion of inflammatory cytokines and middle molecule like beta 2 macroglobulin might have reduced the frequency of cardiovascular morbidity. The dialysis adequacy in the form of weekly KT/V urea in preserved and without preserved RRF group was 2.96 and 3.21 respectively which was statistically non-significant. The entire patient was receiving dialysis through the low flux polysulphone dialyzer.
Both the preserved RRF and without preserved RRF group had significant difference in systolic and diastolic blood pressure. In without preserved RRF group SBP was higher and DBP was lower than the preserved RRF group. Wide pulse pressure was present in without preserved RRF group. This can be explained by more atherosclerosis as the dialysis duration was higher in without preserved group than preserved RRF group (20.95 vs 7.56, p=0.001). Serum calcium, serum phosphate and hemoglobin level was similar in both groups. Similar finding was found in the study of Hwang HS. Serum calcium and phosphate product had an impact on atherosclerosis development and atherosclerosis was an important reason of coronary artery diseases.16 In case of severe anemia heart failure may developed which is detected by low left ventricular EF in echocardiography. Most of the patient had mild to moderate anemia. Without preserved RRF group had 55% moderate anaemia compared to 56.3% of preserved RRF group. The mean Hb was 9.77±1.34 in preserved RRF group and 9.82±1.06 in without preserved RRF group (p=0.841). Higher mean Hb level was found in several studies16‒18,23 Levels of Hb in HD patients is associated with several complications such as cardiovascular disorders, dysrhythmias and cardiac hypertrophy, stroke, and arteriovenous fistula dysfunction.24 Anemia increases the risk of hospitalization, morbidity, and mortality in Hemodialysis patients.25,26
Both the preserved and without preserved RRF group in HD had statistically significant difference in dialysis duration (7.56±8.13 vs 20.95±14.20, p<0.001). Longer duration of dialysis as a consequence, gradually reduce the urine output. Dialysis blood flow was statistically non-significant in both the preserved and without preserved RRF (229.69±21 vs 229.5±20.9, p=0.970). Similar loss of residual function was seen in a study done by zhanget al.27 BMI was also non-significant in preserved and without preserved RRF group. Mean BMI in preserved RRF and without preserved RRF was 23.07±4.36 and 21.30±3.51, p=0.061 respectively. Lower body weight might have an impact on cardiovascular morbidity as seen in this study. Similar findings were reported in several studies. Higher body mass was paradoxically associated with better survival. 16,26 In this study demonstrated the inferior cardiovascular morbidity in patients with reserved RRF undergone twice weekly or thrice weekly HD compared with patient without RRF. The result of this study was similar with the study done by Hwang HS et al.16 In regression analysis it was seen that RRF, age and dialysis duration had a statistically significant relation with cardiovascular morbidity. No significant relation was seen between BMI, DM, HTN, serum lipid and cardiovascular morbidity.
In this study, preserved RRF were significantly associated with less frequent diastolic dysfunction, left ventricular hypertrophy and higher level of left ventricular ejection fraction compared to without preserved residual renal function. So, there was significant relation of residual renal function with cardiovascular morbidity.
The present study has got some limitations. 24 hours urine collection might not be accurate as the patient collected their urine at home during inter-dialytic period. Sample size was limited that may not reflect the whole scenario.
The findings of this study suggest that careful selection of the patient to preserve the residual renal function in Hemodialysis as long as possible. However, further large-scale multicenter study is recommended to validate the findings of the study.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
- 1. Schieppati A, Remuzzi G. Chronic renal diseases as a public health problem: epidemiology, social, and economic implications. Kidney Int Suppl. 2005;68(98):S7–S10.
- 2. Centers for Disease Control and Prevention. Chronic Kidney Disease Surveillance System—United States. 2015.
- 3. Hyodo T, Hirawa N, Hayashi M, Than KMM, Tuyen DG, et al. Present status of renal replacement therapy at 2015 in Asian countries (Myanmar, Vietnam, Thailand, China, and Japan). Renal Replacement Therapy. 2017;3(11):1–14.
- 4. Vanholder R, Laecke SV, Verbeke F, Glorieux G, Biesen WV. Uraemic toxins and cardiovascular disease: in vitro research versus clinical studies. NDT Plus. 2008;1(1)2–10.
- 5. Kanbay M, Afsar B, Goldsmith D, Covic A. Sudden death in hemodialysis: An update. Blood Purif. 2010; 30(2):135–145.
- 6. Dai L, Golembiewska E, Lindholm B, Stenvinkel P. End-stage renal disease, inflammation and cardiovascular outcomes. Contrib Nephrol. 2017;191:32–43.
- 7. Termorshuizen F, Dekker FW, Van-Manen JG, Korevaar JC, Boeschoten EW, et al. NECOSAD Study Group: Relative contribution of residual renal function and different measures of adequacy to survival in hemodialysis patients: an analysis of the Netherlands Cooperative Study on the Adequacy of Dialysis (NECOSAD)-2. J Am Soc Nephrol. 2004; 15(4):1061–1070.
- 8. Kalantar-Zadeh K, Unruh M, Zagan PG, Kovesdy CP, Bargman JM, et al. Twice-weekly and incremental hemodialysis treatment for initiation of kidney replacement therapy. Am J Kidney Dis. 2014;64(2):181–186.
- 9. Brener ZZ, Kotanko P, Thijssen S, Winchester JF, Bergman M. Clinical benefit of preserving residual renal function in dialysis patients: an update for clinicians. Am J Med Sci. 2010; 339(5):453–456.
- 10. Hemodialysis Adequacy Work Group. Clinical practice guidelines for hemodialysis adequacy. Am J Kidney Dis. 2006;48(1):S2–90.
- 11. Lin X, Yan Y, Ni Z, Gu L, Zhu M, et al. Clinical outcome of twice-weekly hemodialysis patients in shanghai. Blood Purif. 2012; 33(1-3):66–72.
- 12. Hanson JA, Hulbert-Shearon TE, Ojo AO. Prescription of twice-weekly hemodialysis in the USA. Am J Nephrol. 1999;19(6):625–633.
- 13. Wang AYM, Lai KN. The importance of residual renal function in dialysis patients. Kidney Int. 2006; 69(10):1726–1732.
- 14. Mathew AT, Fishbane S, Obi Y, neck G, Angeless L. Preservation of Residual Kidney Function in Hemodialysis Patients: Reviving an Old Concept for Contemporary Practice. HHS Public Access. 2018;90(2): 262–271.
- 15. Leypoldt JK. Urea standard Kt/V(urea) for assessing dialysis treatment adequacy. Hemodial Int. 2004;8(2):193–197.
- 16. Hwang HS, Hong YA, Yoon HE, Chang YK, Kim SY, et al. Comparison of clinical outcome between twice-weekly and thrice-weekly hemodialysis in patients with residual kidney function. Medicine Baltimore. 2016;95(7):e2767.
- 17. Raikou VD, Kardalinos V, Kyriaki D. The Relationship of Residual Renal Function with Cardiovascular Morbidity in Hemodialysis Patients and the Potential Role of Monocyte Chemo attractant Protein-1. Kidney Dis Basel. 2018; 4(1):20–28.
- 18. Bravo-Jaimes K, Whittembury A, Santivañez V. High prevalence of cardiovascular disease in end-stage kidney disease patients ongoing hemodialysis in Peru: Why should we care about it?. Int J Nephrol. 2015;4–9.
- 19. Saeed A, Bjorkander E, Carlstrom J, Guron G, Kashioulis P, et al. Hemodialysis twice versus three times a week in patients with residual kidney function: quality of life, cardiovascular outcomes and mortality, Regional activity-based HTA. 2014; p 76.
- 20. Huang SH, Filler G, Lindsay RM: Residual renal function calculated from serum cystatin C measurements and knowledge of the weekly standard Kt/V urea. Perit Dial Int 2012; 32(1):102–104.
- 21. Shafi T, Jaar BG, Plantinga LC, Fink NE, Sadler JH, et al. Association of residual urine output with mortality, quality of life, and inflammation in incident hemodialysis patients: the Choices for Healthy Outcomes in Caring for End-Stage Renal Disease (CHOICE) study. American Journal of Kidney Diseases. 2010; 56(2):348–358.
- 22. Mukherjee T, Devi G, Geetha S, Anchan N J, Subbaiyan S S. A comparison of practice pattern and outcome of twice-weekly and thrice-weekly hemodialysis patients. Indian J Nephrol 2017;27(3):185–189.
- 23. Sadeghi M, Ebrahimi H, Abbasi M, Norouzadeh R. Relationship between anemia, quality of life, and laboratory indices in hemodialysis patients. Saudi J Kidney Dis Transpl 2016;27(5):1063–1067.
- 24. DeVita MV, Frumkin D, Mittal S, Kamran A, Fishbane S, et al. Targeting higher ferritin concentrations with intravenous iron dextran lowers erythropoietin requirement in hemodialysis patients. Clin Nephrol 2003;6(5):335–40.
- 25. Locatelli F, Conte F, Marcelli D. The impact of haematocrit levels and erythropoietin treatment on overall and cardiovascular mortality and morbidity - The experience of the Lombardy Dialysis Registry. Nephrol Dial Transplant 1998;13(7):1642–1644.
- 26. Park J, Ahmadi SF, Streja E, Molnar MZ, Flegal KM, , et al. Obesity paradox in end-stage kidney disease patients. ProgCardiovasc Dis. 2014;56(4):415–425.
- 27. Zhang M, Wang M, Li H, Yuan L, Hao C, et al. Association of initial twiceweekly hemodialysis treatment with preservation of residual kidney function in ESRD patient. Am J nephrol. 2014;40(2):140–150.

