Introduction: Non-invasive ventilation (NIV) is a therapeutic option that has been widely used in the treatment of acute respiratory failure in critically ill patients in recent decades. Pressure injuries (PI) of the face are one of the most frequent complications associated with the practice of NIV.
Aim: to characterize patients undergoing NIV who developed PI on the face in the Intensive Care Unit (ICU) of Dr. Nélio Mendonça Hospital (NMH) and determine the incidence and prevalence of PI in patients undergoing NIV in the NMH ICU.
Methods: exploratory retrospective analytical cohort study, with the following inclusion criteria: adults admitted to the ICU for a period of two hours or more and with intact skin at admission, from January 1, 2020 to December 31, 2022.
Results/discussion: In the last three years, 133 patients underwent NIV in the NMH ICU, of which five obtained PI on the face, all of which occurred in males. Ages ranged from 55 to 79 years old. The number of hours under NIV varied between 26 and 111 hours, corresponding to between 2 and 8 days. The incidence of PI on the face was 3.9%, 2% and 6.3% in 2020, 2021, 2022 respectively. The prevalence was 4%.
Keywords: Pressure injury, Non invasive ventilation, Face intensive care unit
The use of Non-Invasive Ventilation (NIV) has been a growing trend in recent decades in the treatment of acute respiratory failure, constituting a therapeutic option in which a mask is used to administer positive pressure ventilation.1
One of the most serious complications resulting from the use of NIV is the development of Pressure Injuries (PI) on the face,2 which are considered a public health problem and are a relevant indicator of the quality of nursing care provided.3 Caring for a patient undergoing NIV in an Intensive Care Unit (ICU) while preserving the skin integrity of the face is an ongoing challenge for nurses.
With this in mind, the aims of this study are to characterize the patients undergoing NIV who developed PI on the face in the ICU of the Dr. Nélio Mendonça Hospital (NMH) and to determine the incidence and prevalence of PI in patients undergoing NIV in the ICU of the NMH.
In order to contextualize the subject under study, bibliographic research was carried out in the Scientific Library On-line (Scielo), B-on EBSCO, Pubmed and Medline electronic databases, using as a reference matrix the fact that evidence-based practice is an approach that leads to the development and/or use of research results in clinical practice. Next, the existing data in the NMH ICU database was consulted.
Respiratory diseases are the leading cause of hospitalization and the third leading cause of death in Portugal according to the National Observatory of Respiratory Diseases (2022) and influence the quality and life expectancy of the population.4
A person with an altered breathing pattern has an inspiration/expiration that does not provide adequate ventilation for effective life support and can be characterized by dyspnea, tachypnea, use of accessory respiratory muscles, cyanosis and changes in gas exchange. These changes can lead to the need for invasive or non-invasive ventilatory support.5
The advantages of NIV are a reduction in the incidence of nosocomial respiratory infection, the need for tracheotomy, prolonged oxygen therapy, parenteral nutrition, length of stay in the Intensive Care Unit, treatment-related costs and improved perception of the state of health of the person in critical condition compared to invasive mechanical ventilation, especially in acute hypoxemic or hypercapnia respiratory failure.6
PI at the site of greatest pressure and skin interface contact is the most documented complication associated with the practice of NIV.7 According to Alqahtani,8 the damage that occurs on the skin associated with the NIV device usually takes the form of the device, and is caused by the pressure it exerts on the skin, which compromises the supply of nutrients and oxygen to the capillaries, causing tissue ischemia.
PI represents a person-centered health problem to which nursing care is sensitive, contributing to health gains and cost optimization; preventive attitudes are therefore essential.
The specialized knowledge of nurses specializing in medical-surgical nursing (MSSN) in intensive care units is essential for the prevention of PI associated with medical devices, as they spend the most time with the patient and play a fundamental role in their monitoring/surveillance.9,10
The exercise of the MSSN must be guided by guidelines based on "evidence" derived from "research results" to guarantee the quality and safety of the care provided.11
In this context, the MSSN plays a key role in identifying the risk factors that can lead to PI on the face and establishes an intervention plan aimed at preventing complications.
In Portugal, the prevention of PI as an improvement in the quality of healthcare is one of the priorities of the General Health of Portugal, which is included in the National Plan for Patient Safety (NPPS) 2021-2026, approved by Normative Order 9390/2021 and which is an important support document for managers and clinicians in the application of good practices in patient safety.12 This plan follows the recommendations of the Council of the European Union of 9 June 2009 on patient safety and is part of a public policy to prevent safety incidents associated with the provision of healthcare within the National Health Service (SNS).
The design of the NPPS 2021-2026 also took into account the recommendations stemming from the United Nations' Sustainable Development Goals, specified in the third goal (health and well-being) and, more recently, the WHO's Global Action Plan for Patient Safety 2021-2030, which emphasized the need for patient safety to be part of the health policy agenda, making it a guiding principle for all national plans to be developed in this area.
This plan envisages that by 2026, 90% of healthcare institutions will be using tools to control and monitor safe practice in relation to the occurrence of pressure injuries.
With this goal in mind and considering the increasing use of this ventilation technique, it is important to assess the impact of PI on the face as a frequent complication resulting from the use of NIV in the critically ill.
The methods used was an exploratory retrospective analytical cohort study, for the period from January 1, 2020 to December 31, 2022. The following inclusion criteria were defined to obtain the sample: adults hospitalized in the NMH ICU for more than 24 hours with NIV for a period equal to or greater than two hours and with intact facial skin upon admission. All participants hospitalized during the study period and who met the previously defined criteria were included in the study. The data for characterizing patients: age, gender, NIV time in days and hours, were obtained from the database of patients undergoing NIV existing in the ICU in digital format with the consent of the service manager.
In the analysis and processing of data, the principles of anonymity and data confidentiality were respected. The results were interpreted using graphs and descriptive statistics.
According to Menoita,13 with the SARS-CoV2 pandemic, there was an increase in the number of patients requiring intensive care, with prolonged hospitalizations, with one or more medical devices, with an expected increase in the incidence of Pressure Ulcers Associated with Medical Devices.
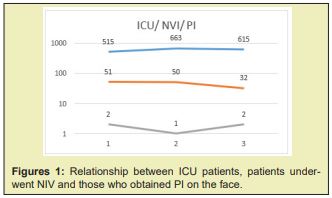
In our study we can see that in the last three years there has been an expected increase in patients admitted to the ICU due to the previously mentioned pandemic from 515 patients in 2020 to 615 in 2022, with a peak inflow in 2021 of 663 patients. However, despite this inflow, patients undergoing NIV have been decreasing, from 51 patients in 2020 to 32 patients in 2022. PI on the face associated with NIV have remained stable, varying between one and two cases per year, making a total of five patients with PI on the face in the last three years, as we can see in Figure 1.
In order to characterize our sample, we can verify that of the 133 patients undergoing NIV in the ICU, 80 are male, making up 60% of our sample and the rest are female, that is, 53 patients, which makes up the remaining 40%. of our sample Figure 2.

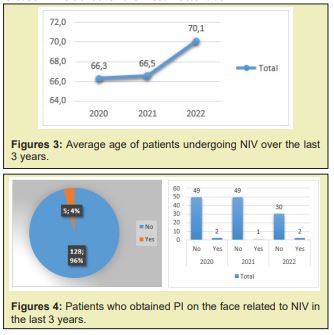
Maintaining the initial premise of characterizing the population that undergoes NIV in the ICU at NMH, we analyzed the average age over the last three years. We found that it has been increasing gradually, with a significant increase of almost four years, between 2020 and 2022, from 66 to 70 years Figure 3.
After characterizing the patients undergoing NIV in the NMH ICU, we aimed to determine the incidence and prevalence of PI on the face of patients undergoing NIV in this ICU, as such, we found that in 2020 of the 49 patients undergoing NIV, two obtained PI on the face, in 2021 of the 49 patients who underwent NIV, one obtained PI on the face and finally, in 2022 of the 30 patients who underwent NIV, two obtained PI on the face Figure 4. Thus, we attest that the prevalence of PI on the face in this ICU is 4% and the incidence varies depending on the years of study. In 2020 the incidence was 3.9%, in 2021 it was 2% and in 2022 it was 6.3%. However, it is worth noting that although statistically there was a significant increase in the incidence of PI on the face in this ICU, when we analyze the actual number of patient’s we find that in 2022 there was a decrease in patients undergoing NIV (51 to 32) and an increase in patients with PI on the face (1 to 2) which justifies this apparently very significant increase in incidence for the most inattentive.
In a 2019 systematic review and meta-analysis, in more than 126,000 patients in 29 studies, the prevalence and incidence of Medical Device- Associated Pressure Ulcers was 12% and 10%, respectively. According to the European Pressure Ulcer Advisory Panel/National Pressure Ulcer Advisory Panel/ Pan Pacific Pressure Injury Alliance,14 in a prevalence study carried out in 2017, 35% to 50% of PI detected were associated with a medical device.
At a national level, a study carried out by Quitério, Cordeiro & Pereira15 in an intermediate care unit at Hospital de Setubal determined an incidence of 14.6% of PI associated with NIV and another study carried out by Machado,16 in an intermediate care unit in the North of Portugal it was 2.5%. It is worth noting that the Spanish Society of Intensive Medicine and Coronary Units (SCIMCI) recommends, as a quality criterion, that the incidence be less than 7%.17
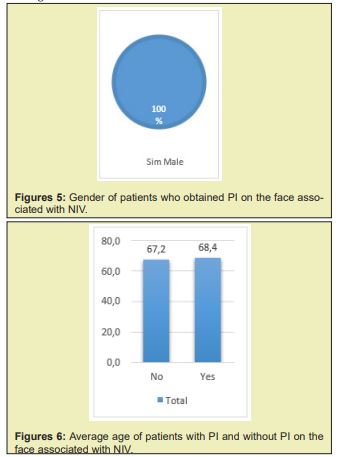
After determining the incidence and prevalence of PI on the face associated with NIV in this ICU, we began to characterize our sample. We determined that PI on the face associated with NIV occurred entirely in males over the last three years Figure 5 and those ages varied between 55 and 79 years, with the average age being 68 years. We also determined that patients who acquired PI on the face are on average 1 year older than the population who did not acquire them Figure 6.
According to the NPUAP, the risk factors for the appearance of PI are: altered perfusion and oxygenation, nutritional deficit, increased skin moisture, increased body temperature, advanced age, altered sensory perception, hematological changes and changes in health conditions.14
Maruccia add that with age the skin loses elasticity, thickness and resistance, making it more vulnerable when subjected to pressure or aggression, thus increasing the risk of PI.18
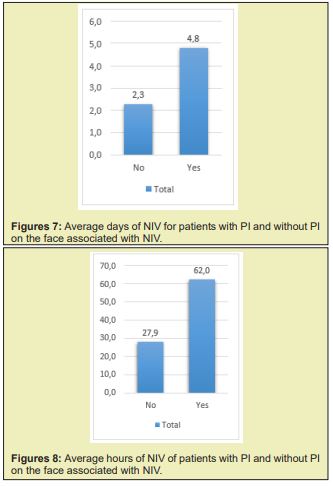
The patients who acquired PI on the face, we found that they used on average around 5 days of NIV, while those who did not acquire it was 2 days of NIV, in other words they used NIV more than twice as many days of NIV Figure 7. The same was true when we analyzed the number of hours that patients underwent NIV. Patients who acquired PI on the face performed an average of 62 hours of NIV, while those who did not acquire PI performed an average of 28 hours, that is, they performed more than twice as many hours of NIV Figure 8. Thus, we found a direct relationship between the number of hours and days of NIV with the acquisition of PI on the face.
A retrospective analytical cross-sectional study, which analyzed data from 600 patients admitted to an Intermediate Emergency Care Unit in a Hospital Center in the North of Portugal, determined that patients undergoing a greater number of NIV days and a greater number of days of hospitalization presented higher frequency of development of PI, in line with the results of our study.16,19-21
The PI are a public health problem, an indicator of the quality of nursing care provided and constitute a recurring problem in Portugal. The General Health in Portugal in 2011 states that the prevention of PI is the most effective element and it is estimated that 95% of PI can be prevented, with this responsibility being up to nurses.
In this study we can conclude that although the number of people attending the SMI is increasing, the number of patients undergoing NIV has been decreasing and PI associated with NIV has remained stable. The incidence of PI in our study was 3.9%, 2% and 6.3% in 2020, 2021, 2022 respectively. The prevalence was 4%. The number of hours and days with NIV increased the frequency of PI.
In this study, it is estimated that the low incidence and prevalence of PI on the face associated with NIV is due to the working method of the responsible nurse who applies the individualized nursing process to each patient, with the following nursing interventions: choose the appropriate size of the NIV mask, monitor the skin at the interface application site every two to four hours, avoid excessive tightening of the interface, ease the mask every two hours taking into account the patient's health status, apply fatty acids hyperoxygenated, maintain normothermia, keep the skin clean and dry, provide adequate nutrition, assess pain, and a standard procedure was created that could be extended to the entire nursing team.
There is also a nurse in this ICU responsible for monitoring, controlling and auditing PIs in this service annually, using a digital tool to record them. Annually, PI data is analyzed by this responsible nurse and presented to the team, discussing the best intervention strategies, thus making the team more effective and competent, in line with what is recommended by the Portuguese National Plan for Patient Safety 2021-2026.
A shortcoming of this study was that it was not possible to understand which nursing interventions had the greatest impact on the incidence of PI, once the standard procedure was implemented.
Assessing the risk of developing PI is fundamental in planning and implementing measures for its prevention and treatment (General Health in Portugal, 2011).
Therefore, in the incessant search for continuous improvement in the prevention of PI on the face associated with NIV, it is recommended to apply the Braden Scale upon admission to the ICU and its reassessment every 24 hours as recommended by the General Health in Portugal (2011), as well as assessing the patients' level of dependence, using the Barthel Index, and the state of consciousness using the Glasgow Coma Scale, since the lower the score on these scales, the greater the probability of acquiring PI.
None.
None.
The author declares no conflicts of interest regarding the publication of this paper.
- 1. Cammarota G, Simonte R, De Robertis E. Comfort During Non-invasive Ventilation. Front Med (Lausanne). 2022;9:874250.
- 2. Wu PL, Li YJ, Pai HC, et al. Factors associated with facial pressure injury in patients receiving non-invasive positive pressure ventilation mask: A retrospective case-control study. J Clin Nurs. 2022.
- 3. General Health in Portugal. Escala de Braden: Versão Adulto e Pediátrica (Braden Q). Orientação n.º17. Lisboa. Ministério da Saúde. 2011.
- 4. Observatório Nacional das Doenças Respiratórias. 15ª Relatório. Fundação Portuguesa do Pulmão. 2022.
- 5. Arsude S, Sontakke A, Jire A. Outcome of Noninvasive Ventilation in Acute Respiratory Failure. Indian J Crit Care Med. 2019;23(12):556-561.
- 6. Ergan B, Nasiłowski J, Winck JC. How should we monitor patients with acute respiratory failure treated with noninvasive ventilation?. Eur Respir Rev. 2018;27(148):170101.
- 7. Wei Y, Pei J, Yang Q, et al. The prevalence and risk factors of facial pressure injuries related to adult non-invasive ventilation equipment: A systematic review and meta-analysis. Int Wound J. 2023;20(3):621-632.
- 8. Alqahtani JS, AlAhmari MD. Evidence based synthesis for prevention of noninvasive ventilation related facial pressure ulcers. Saudi Med J. 2018;39(5):443-452.
- 9. Peña Otero D, Salvà Costa V, Esquinas Rodríguez AM. Cuidados de enfermería en la instauración y mantenimiento de la Ventilación Mecánica No Invasiva. Revisión bibliográfica narrative. Enfermería Activa. 2019;XII:5-26.
- 10. Lin F, Wu Z, Song B, et al. The effectiveness of multicomponent pressure injury prevention programs in adult intensive care patients: A systematic review. Int J Nurs Stud. 2020;102:103483.
- 11. Despacho Normativo nº 429/2018 da Ordem dos Enfermeiros. Diário da República: II Série, nº 135. 2018.
- 12. Despacho Normativo nº 9390/2021 do Ministério da Saúde. Diário da República: II Série, nº 28. 2021.
- 13. Menoita E. Device-related pressure ulcers in Patients and Healthcare Professionals. Journal of Aging & Innovation. 2020;9(2):48-66.
- 14. National Pressure Ulcer Advisory Panel. Pressure Ulcer Stages. 2015
- 15. Quitério C, Cordeiro I, Pereira M. Associated factors of facial pressure ulcers in patients under non-invasive ventilation during hospital stay in an intermediate care facilities of a Portuguese hospital. A Nursing Practice Today. 2020;7(2):97-105.
- 16. Machado I, Monteiro J, Correia T, et al. Úlceras de pressão na face em doentes submetidos a ventilação não invasiva. In VI Encontro de Jovens Investigadores, Bragança. 2019.
- 17. Spanish Society of Intensive Medicine and Coronary Units (SCIMCI). Indicadores de Calidad Del Enfermo Crítico - Actualización 2017.
- 18. Maruccia M, Ruggieri M, Onesti MG. Facial skin breakdown in patients with non-invasive ventilation devices: report of two cases and indications for treatment and prevention. Int Wound J. 2015;12(4):451-455.
- 19. Kottner J, Cuddigan J, Carville K, et al. Prevention and treatment of pressure ulcers/injuries: The protocol for the second update of the international Clinical Practice Guideline 2019. J Tissue Viability. 2019;28(2):51-58.
- 20. Gefen A, Ousey K. Update to device-related pressure ulcers: SECURE prevention. COVID-19, face masks and skin damage. J Wound Care. 2020;29(5):245-259.
- 21. Portaria n.º 22/2023, do Ministério da Saúde. Diário da República: I Série nº5. 2023.

