Introduction: Antibiotics constitute a pillar in the care of pediatric patients who attend hospital institutions.
Objective: To characterize the use of antibiotics in hospitalized patients in the Pediatric Service of the General Teaching Hospital “Cptan. Roberto Rodríguez Fernández” from Morón, in the Ciego de Ávila province.
Methods: A cross-sectional descriptive study was carried out between January and December 2019 in a total of 1,237 pediatric patients who met the inclusion criteria. Data were extracted from individual medical records. Ethical principles for human research were met.
Results: In less than a quarter (22,73%) of the patients, antimicrobial therapy was applied supported by previous microbiological results. Ceftriaxone was the most widely used antibiotic (41,23%); Cefotaxime (16,57 %) and trifamox (12,21 %) followed in order.
Conclusion: Third generation cephalosporins were the most widely used antibiotics. Microbiological studies prior to drug administration were low.
Keywords: Anti bacterial agents/Therapeutic use; Drug prescriptions; Cephalosporins/Therapeutic use
With the discovery, by Fleming, of penicinilla in 1928, the so-called era of antibiotics began. From that date, there was an exponential increase in the creation of new classes of these agents, especially in developed countries. The introduction of antibiotics generated a significant reduction in morbidity and mortality from infectious diseases, and prolonged the life expectancy of the population.1
The use of antibiotics in clinical practice was one of the greatest advances in medicine, both for its direct effects (curing infections) and indirect effects (development of therapeutic procedures –associated with a high probability of the appearance of serious infections–, such as transplants, mechanical ventilation, etc.). In fact, this period in the history of medicine has been called, by some authors, the “antibiotic era”.1
The most striking expression of the positive effect of antimicrobials is observed in patients with severe infections (severe sepsis and septic shock). In these cases, the early use of appropriate antibiotics is associated with very marked benefits in terms of mortality reduction; no other therapeutic intervention in medicine has such an impact.2
Antimicrobials are a therapeutic resource frequently used in health institutions for the prevention and control of infectious diseases. This measure generates problems that, over time, have become more complex due to growing antimicrobial resistance and the costs of new drugs.3
There are precedents on studies on the prescription of antibiotics in pediatric ages both in Cuba and internationally;4,5 however, there are no known recent works on this problem in the General Hospital of Morón. This work constitutes a first approach to this subject that is part of a research project, approved by the Department of Science and Technology of the Faculty of Medical Sciences of Morón.
The objective of this work is to characterize the use of antibiotics in patients hospitalized in the Pediatric Service of the General Teaching Hospital “Cptan. Roberto Rodríguez Fernández” from Morón, province of Ciego de Ávila.
A cross-sectional descriptive study was carried out in the period between January and December 2019. We worked with the 1,237 pediatric patients who received antibiotic treatment during the study period. This represented all those admitted to the Pediatric Service of the General Hospital of Morón, who met the following inclusion criteria: admitted pediatric patient whose disease that led to admission required antibiotic treatment, signature of informed consent by the parents or guardians, and medical history. updated individual clinic.
Data were obtained from individual medical records, and summarized in a form prepared by the author. Descriptive statistical methods were applied that allowed the analysis, interpretation and presentation of the information. For this, tables with absolute and relative frequencies were used.
Throughout the investigation, the ethical principles defined in the Declaration of Helsinki were complied with.6 The author was always careful not to divulge the identity data of those investigated.
Of the total number of patients, only 281 (22.73%) received antimicrobial therapy based on previous microbiological results Table 1.
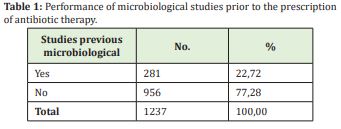
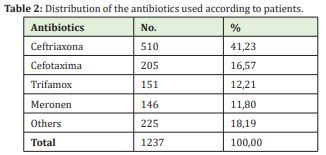
Table 2 shows the most commonly used antimicrobials during the research period. Ceftriaxone was the most used (41.23%); Cefotaxime (16.57%) and Trifamox (12.21%) followed in order of frequency. ceftriaxone was the most used (41.23%); Cefotaxime (16.57%) and Trifamox (12.21%) followed in order of frequency.
There is no doubt that a certain number of patients require therapy without microbiological support, due to urgency or the intensity of the clinical picture. The results of this study correspond to those of other authors.7,8
According to Chaves-Ribeiro and Costa-Aguiar,9 hospital infections are, in particular, a great challenge for health professionals who work in child care. This is due to its extreme fragility, and the potential risk that any medical or surgical action or intervention represents for your health.
Worldwide, both infections and the widespread use of antimicrobials have become a serious problem in pediatric patients, due to the morbidity and mortality associated with the infectious process, and the consequences that the use of antibacterials implies.10 For For this, it is necessary to know, in each healthcare center, the microorganisms most commonly causing sepsis, the patterns of antimicrobial resistance, and the updated therapeutic protocols. Only then can more effective strategies be implemented to control infections acquired during the hospital stay, and guarantee the rational use of antibiotics.11
Respiratory sepsis and urinary tract infections are the first two causes of admission to the Pediatric Service, which entails a high use of cephalosporins. In both diseases, according to the current protocols at the General Hospital of Morón, ceftriaxone is the antibiotic of choice for treatment. A high incidence of soft tissue infections, acute otitis media, and meningitis was also identified, for which third-generation cephalosporins –specifically ceftriaxone– are the antibiotic of choice. These results correspond to those found in other investigations.5,12
A study conducted at the "Dr. Juan de la Cruz Martínez" North Teaching Children's Hospital in Santiago de Cuba included 1,311 patients who received antimicrobials. Ceftriaxone was the most commonly used medication (64.80% of cases) and bacterial pneumonia was the most frequent condition.5
Regarding the use of antibiotics, Fariña –as quoted and reaffirmed by Serra-Valdés–13 refers that the excessive use of antibiotics is one of the factors that contributes to the increase in the resistance of bacteria to these drugs. This is due to the development of strains whose mechanisms of resistance to antibiotics reduce the possibilities of effective treatment of communicable diseases, increase the use of expensive drugs, prolong hospital stay, and increase the risk of mortality. These problems, in the author's opinion, should be avoided through the rational use of antibiotics in hospital institutions, with compliance with the antimicrobial policy, the actions emanating from the pharmacotherapeutic committees and, specifically, from the antibiotic committee of each care unit.
The present investigation had as limitations that sociodemographic variables were not included, and the insufficient inquiry about others of a clinical-pharmacological nature.
Third-generation cephalosporins were the most widely used antibiotics in the treatment of pediatric patients admitted to the General Teaching Hospital of Morón, but the performance of previous microbiological studies was low. The contribution of the research lies both in the increase of scientific evidence on the subject, as well as in serving as support to carry out analytical and other studies, linked to the rational use of medicines.
None.
None.
The authors declare no conflict of interest.
- 1. Cook JH. Uso racional de antibióticos en México. Rev Mex Cienc Farm. 2018;41(2):5-6.
- 2. Bustos R. Shock séptico en pediatría: menos, es más. Rev chil Pediatr. 2016;87(2):148-150.
- 3. Ortiz Ibarra FJ, Morales Méndez I, Gil Acevedo A, et al. El reto de la resistencia bacteriana en México: los beneficios de contar con una nueva alternativa de manejo antimicrobiano eficaz. Med Int Mex. 2009; 25(5):361-371.
- 4. Deresinski S. Principles of antibiotic therapy in severe infections: optimizing the therapeutic approach by use of laboratory and clinical data. Clin Infect Dis. 2007;45:S177-S183.
- 5. Mengana López E, Pérez Reyna, Menéndez Rodríguez M, et al. Uso de antimicrobianos de amplio espectro en un hospital pediátrico de Santiago de Cuba. MEDISAN. 2012;16(9):1341-1349.
- 6. Asociación Médica Mundial. Declaración de Helsinki de la AMM. Principios éticos para las investigaciones médicas en seres humanos. Ratificada en la 64ª Asamblea General, Fortaleza, Brasil, octubre 2013. Helsinki: 18ª Asamblea Mundial; 1964.
- 7. Ruvinsky S, Mónaco A, Pérez G, et al. Motivos de la prescripción inade- cuada de antibióticos en un hospital pediátrico de alta complejidad. Rev Panam Salud Pública. 2011;30(6):580-585.
- 8. Boutal H, Vorgel A, Bernabeu S, et al. A multiplex lateral flow immunoassay for the rapid identification of NDM-, KPC-, IMP-and VIM-type and OXA-48-like carbapenemase-producing Enterobacteriaceae. J Antimicrob Chemother. 2018;73(4):909-915.
- 9. Chaves Ribeiro I, Costa Aguiar BG. Factores intrínsecos predisponentes a infección hospitalaria y a óbito neonatal. Enferm Glob. 2013;12(30).
- 10. Urzúa S, Ferrés M, García P, et al. Estrategias para reducir infecciones, uso de antimicrobianos y sus efectos en una unidad de neonatología. Rev chil infectol. 2017;34(2):99-107.
- 11. Paris Licorish M, Mariño Castellanos MC, Maceira Soto Z, et al. Caracterización clínica y microbiológica de niños y adolescentes con infecciones asociadas a la atención sanitaria. MEDISAN. 2018;22(5):508-517.
- 12. González Rubio R, Parra Blázquez D, San Juan Sanz I, et al. Evolución de la incidencia de pacientes con colonización e infección por bacterias productoras de carbapenemasas VIM en un hospital pediátrico en España. Rev Esp Quimioter. 2019;32(1):60-67.
- 13. Serra Valdés MA. La resistencia microbiana en el contexto actual y la importancia del conocimiento y aplicación en la política antimicrobiana. Rev haban cienc méd. 2017;16(3):402-419.

