Spontaneous intracerebral hemorrhages constitute an entity with high mortality within cerebrovascular diseases at the General Provincial Teaching Hospital "Capitán Roberto Rodríguez Fernández". There are well-established prognostic criteria, but most of them are based on clinical elements.
Objective: To determine morphometric predictors of mortality in patients with spontaneous lobar intracerebral hemorrhage.
Methods: A prospective correlational study was carried out.
Results: Morphometric analysis of the tomographic images of spontaneous lobar intracerebral hemorrhages was carried out and the morphometric variables were correlated with the state at hospital discharge of the patients to determine the morphometric predictive indicators of mortality.
Conclusions: The determined morphometric indicators made it possible to identify the patients with the highest risk of mortality due to spontaneous lobar intracerebral hemorrhage.
Keywords: Intracerebral hemorrhages, Morphometric indicators, Mortality, Older adult
The presence of blood in the parenchyma is called cerebral or intraparenchymal hemorrhage. If it breaks into the cerebral ventricles it is called intraventricular hemorrhage, if its presence is in the subarachnoid space; subarachnoid hemorrhage, and if there is blood in the brain parenchyma and subarachnoid space then it is called cerebromeningeal hemorrhage.
Spontaneous intracerebral hemorrhage (ICH) is a health problem for humanity and constitutes a challenge for the international medical community. HICE is suffered by around two million people each year worldwide.1-3
The prognostic variables related to short-term mortality from ICH are diverse and in many cases inconsistent, due to their variation from one study to another.4-7 However, the following are cited as independent prognostic factors: the initial Glasgow Coma Scale (GSC) value, the volume of hemorrhage, intraventricular extension, the patient's age, association with hydrocephalus, perihematoma edema, and presence of coagulation disorders.
In Cuba, some studies have been carried out to determine factors with prognostic value in patients with HICE. Pérez Pupo4 in the study "Mortality from cerebrovascular diseases" carried out in 2007 point to cerebral edema as the factor most associated with mortality from HICE.
Barrios Fuentes5 in the article "Tomographic findings and mortality in patients with spontaneous intracerebral hemorrhages", carried out in 2010, found that the factors most related to mortality were: advanced age, non-white skin color, presence of hydrocephalus , displacements of midline structures greater than 5mm. In another investigation carried out in 2012, Aguilera Pacheco6 demonstrated that there is a directly proportional relationship between the volume of hemorrhage greater than 60 mL and the poor prognosis of the patient.
In 2013, Suárez Quesada7 presented the work entitled "Predictors of mortality in spontaneous supratentorial intracerebral hemorrhage" in which the displacement of midline structures ≥ 2.5mm and the score in the Glasgow scale ≤ 12 points as the main predictors related to death.
There are multiple factors that are considered predictors of mortality for patients with spontaneous lobar intracerebral hemorrhage (SILH). These have been shown to be inconsistent from one study to another, which is why it is important to delve into the subject.8
Morphometric indicators have not been used so far in prognostic studies of mortality due to HICLE in patients 60 years of age and older. Therefore, the limitations of other prognostic factors reported in the literature on the subject can be mitigated with the application of these indicators.
With the realization of the morphometric analysis, the dimensions and shape of the HICLE can be determined. Through the variables: area, perimeter, size and volume, the dimensions are established and with the shape factor (elliptical, circular and circulating) the shape of this type of intracranial hemorrhage can be defined. By considering measurable quantitative variables, this analysis improves diagnostic accuracy.
To determine morphometric predictors of mortality in patients aged 60 years and over with HICLE.
Type of study: Prospective correlational.9
Study period: January 2018 – December 2019.
Universe. This is a population made up of 67 patients, whose characteristics are: patients aged 60 years and over with HICLE determined by CT within the first six hours of the onset of symptoms.
Information collection techniques and procedures
The data were captured in a data collection model in the tomography department before and after the examination, in addition the patients' medical records were used. Image interpretations were performed by the imaging specialist.
The measurements were made by the author of the research and the imaging specialists who covered the on-call hours, after training with the MADIP program, given by the main author of the system.
The results of the measurements were included in a database of the SPSS utility, version 15.0, for further analysis and statistical processing.
Information analysis techniques and procedures
The patients were classified into two groups according to their hospital discharge status: alive and deceased. The mean, standard deviation, range, maximum value, and minimum value were calculated for each of the variables. Subsequently, the results in both groups were compared and the confidence intervals for the arithmetic means of each of the morphometric variables were calculated with a reliability level of 95%.
The volume and location of the hematoma, confirmed by CT, are useful data for choosing the surgical option. The patients who benefit the most from the operation are those who show HICLE with a volume of 20 -50cm3; those larger than 60cm3 have a poor prognosis with any type of treatment. Regarding its location, the recommendation is generally restricted to lobar hematomas, but its accessibility is more important.9
There is a better evolution after the operation in patients with hematomas that reach a distance of less than 1cm to the cortical surface. The right temporal location must be individually evaluated, because due to its mass effect on the mesial portion of the temporal lobe and its close relationship with Bichat's cleft, the frequency of herniation of the temporal uncus is greater with lower intracranial pressures. compared to other topographies. The mass effect and the displacement of the midline greater than 5mm demonstrated by the CT should be considered when making decisions.10,11
Morphometric analysis of 67 patients with spontaneous lobar cerebral hemorrhages divided into two groups: 51 alive and 16 deceased. The segmentation of the hemorrhages was performed with the MADIP program and a characteristic vector was obtained for each lesion measured with the values of the following variables: area, perimeter, size, minimum diameter, maximum diameter, elliptical shape factor, circular shape factor, and circulating shape factor.
Table 1 shows the confidence intervals for the morphometric indicators that express the dimensions of the figure to be measured in patients with HICLE. It is observed that the intervals of all the indicators are greater in the group of deceased patients, which shows that the greater the dimension of the HICLE, the greater the probability that the patient will evolve unfavorably and die. Volume is the only morphometric indicator used in the literature to refer to the prognosis of HICLE.1,10
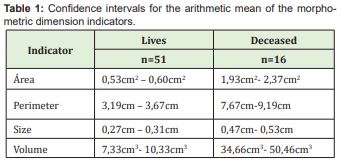
The patients who were discharged deceased presented a confidence interval for the volume between 34.66cm3 and 50.46cm3, lower than the 60cm3 that other authors propose as a predictive criterion for mortality (6.9), but higher than those who survived. This result coincides with the criterion based on the analysis of the Monroe and Kelly doctrine, of the possible directly proportional relationship between volume, intracranial pressure and mortality defended by Lacerda.11
Regarding the rest of the morphometric indicators of dimension, we consider that, together with the volume, these allow to characterize and classify the HICLE with greater accuracy.
The larger the dimensions of a HICLE, expressed by its area, perimeter, volume, and size, the greater the chances that it behaves like an expansive intracerebral process, with a larger area affected and more possibilities for displacement of structures of the brain. midline, which is accepted as a poor prognostic element.10,12
Table 2 characterizes the patients according to the values of the different shape factors and the state at discharge of the patients. According to the MADIP user manual (15), it is considered that the closer to 1 the hemorrhage is rounder and that hemorrhages of 0.8 are considered spherical, it also states that the closer to 0 the hemorrhage is. more elliptical and as can be seen in Table 2, the interval of the elliptical shape value of the deceased was much closer to 0 than in the living graduates. According to the literature reviewed, these shape indicators have not been used before to issue a prognosis for patients with HICLE, although there is reference that HICLE have an elliptical shape.
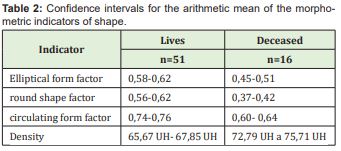
The density value is used in CT to determine the image texture of a structure. Expressed in Hounsfield units (HU), it helps to specify whether a certain structure of the human body is made up of blood, bone, gas or fat, among other substances. In addition, in the case of HICLE, it can guide the time of evolution of the disease, due to the metabolism process suffered by the hemoglobin discharged outside the blood vessels. The more hyperdense the image, the shorter the extravasation time to brain tissue.
In the case of HICLE, it is considered that the normal value should be approximately 60 HU. In the study, it was verified that the confidence intervals of the arithmetic mean of the density presented higher values in the deceased discharged patients, which suggests the possibility of bleeding with a volume sufficient to cause uncontrollable intracranial hypertension events that caused death at these patients early or the occurrence of rebleeding events with growth in the volume of the initial HICLE with the same results, perfectly documented phenomena in the reviewed literatura.8,13,14
The determined chordometric indicators made it possible to identify the patients with the highest risk of mortality due to HICLE.
None.
None.
Authors declares that there is no Conflicts of Interest.
- 1. Rodríguez Yáñez M, Castellanos M, Freijo MM, et al. Guías de actuación clínica en la hemorragia intracerebral. Neurología. 2013;28(4):236–249.
- 2. Lloyd Jones D, Adams RJ, Brown TM, et al. Heart disease and stroke statistics 2010 update: a report from the American Heart Association. Circulation. 2010;121(7):e46–e215.
- 3. Dubourg J, Messerer M. State of the art in managing nontraumatic intracerebral hemorrhage. Neurosurgl Focus. 2011;30(6):E22.
- 4. Pérez Pupo RD, Leyva Rojas KM. Mortalidad por enfermedades cerebrovasculares. Hospital “Vladimir Ilich Lenin”, Holguín. Correo CientífMéd Holguín. 2010;4(2):1.
- 5. Barrios Fuentes PJ, Bernal Muñoz JL, Osorio Pagola MF, et al. Hallazgos tomográficos y mortalidad en pacientes con hemorragias intracerebrales no traumáticas. Medisur. 2011;9(2):1.
- 6. Aguilera Pacheco OR, González Vidal D. Factores pronósticos en la hemorragia cerebral intraparenquimatosa. MEDISAN. 2012;16(1):1.
- 7. Suárez Quesada A, López Espinosa E, García Verdecia N, et al. Predictores de mortalidad en la hemorragia intracerebralsupratentorial Espontánea [CD-ROM]. La Habana: URGRAV. 2017;13(4):397–404.
- 8. Tellería Díaz A. Tratamiento e indicadores pronósticos del paciente con hemorragia intracerebral espontánea. RevNeurol. 2006;42(6):341–349.
- 9. ArtilesVisbal L, Otero Iglesias J, Barrios Osuna I. Metodología de la investigación para las ciencias de la salud. La Habana: Ciencias Médicas; 2009.
- 10. Leira R, Dávalos A, Silva Y, et al. Early neurologic deterioration in intracerebral hemorrhage. Predictors and associated factors. Neurology. 2004;63(3):461–467.
- 11. Lacerda Gallardo AJ, Díaz Agramonte JA, Martín Pardo JC, et al. Resultados de 11 años de tratamiento quirúrgico en las hemorragias intracerebrales lobares espontáneas supratentoriales. Rev Cubana Neurol Neurocir. 2012;2(2):114–120.
- 12. Keep RF, Hua Y, Xi G. Intracerebral haemorrhage: mechanisms of injury and therapeutic targets. Lancet Neurol. 2012;11(8):10.
- 13. Kase CS, Mohr JP, Caplan LR. Intracerebral hemorrhage. In: Barnett HJM, Mohr JP, Stein BM, Yatsu FM, editors. Stroke: pathophysiology, diagnosis and treatment 3rd (edn). New York. 1998:pp.649–700.
- 14. Madip. Análisis morfométrico mediante el procesamiento digital de imágenes. Manual de Usuario. La Habana: ICIMAF; 2019.

