Inpatient falls are the primary cause of injuries in health care facilities. The intended project goal was to reduce inpatient falls in the cardiac step-down unit (CSU). Adding the Medication Fall Risk Score to the current fall risk assessment resulted in fewer falls. The CSU had the highest fall rate and the highest increase in patient falls. Patients in the CSU are often older. Medications used to treat this patient population are betablockers and antihypertensive meds. These medications are in the class of falls risk inducing drugs (FRIDs), which increases the possibility of falls in this population.
Keywords: Inpatient falls, Patient population, CSU, Falls risk inducing drugs
The Cardiac Stepdown Unit (CSU) showed a 51% increase in falls while all other hospital units showed a decrease. Fall rates of the CSU are 4.12 per 1000 patient days which is above the hospital average of 1.89, and the national stepdown unit average of 3.44 (AHRQ, 2022). The CSU falls rate prompted discussion of current practices with the Quality Improvement Coordinator (QIC).1
Current hospital falls prevention protocols include the Hester-Davis Scale for Falls Risk Assessment (HDS), bedside assistance, and hourly rounding which are recommended by the AHRQ.2 Patient education, using brochures, and the teach-back method, is utilized to improve outcomes (Heng, 2020). High-risk patients receive additional bedside assistance depending on the impairment (gait, visual, cognitive).
The Quality Improvement Coordinator (QIC) performed a root cause analysis, and then the project team discussed the results. Nurses followed regular protocols regarding fall prevention, and patients understood their falling risk. According to the QIC, following a review of the medication taken by the patients that experienced a fall, those patients were continuing medication regimens that included FRIDs (J.F. personal communication, March 7, 2021). Analysis of patient vitals determined medication orthostatic hypotension as contributing factor in patients that fell. Therefore, a gap in nursing practice for falls prevention was identified. The Project Manager suggested an update to the assessment criteria for falls risk.
The PICOT question for the project is, “In the Cardiac Stepdown Unit, how does the addition of a Medication Fall Risk Score to the fall prevention protocol affect patient fall and identifying high-risk patients compared to the current falls risk assessment over a 10-week time frame?” Preventing Falls in Hospitals (2018) states that between 700,000 and 1,000,000 patient falls occur yearly.3 Patient falls cause increased costs for the patient and the facility due to increased length of stay.4 The geriatric patient population is at a greater risk for falls and falls with injuries.5
Medications known to increase the risk of patient falls include antipsychotic medications, antihypertensive medications, and opioids.5-9 Side effects from these medications like gait issues, syncope, and postural hypotension, which increase the risk of falling in patients.5-9 The additional risk from fall risk-inducing drugs (FRIDs) can be determined using the Medication Fall Risk Score (MFRS) tool to assess patients.6,8,9 Addressing polypharmacy helps to reduce the chances of inpatient falls, inpatient falls with injuries, increased mortality rates, and increased patient costs.4-6,10,11 However, addressing polypharmacy by deprescribing medications must be done with attention to withdrawal side effects and factors like frailty, which exacerbate the effects of FRIDs.5,11
The experience of an inpatient fall causes feelings of stress, anxiety, and loss of confidence in patients after the occurrence.12,13 Educating patients on fall prevention techniques and their risk factors helps prevent falls.12,13 Staff education using a team-based approach is beneficial because different departments are trained simultaneously.14-16
Bromfield et al.5 linked indicators of frailty, which include a previous history of falls, exhaustion, depressive symptoms, and cognitive impairment, to an increase in falls for geriatric patient populations. The article also stated that after multivariate analysis, an increased fall risk did not result from polypharmacy, antihypertensive medications, systolic blood pressure (SBP), or diastolic blood pressure (DBP).5 The article suggests that frailty indicators, along with FRIDs, must be part of the fall evaluation criteria.
Reducing Polypharmacy
Many patients that suffer inpatient falls were taking multiple medications at the time of their fall.5-9,11,17 Researchers cite polypharmacy as hindering the quality of life, increasing the chance of falls with injuries, increasing patient costs, and increasing mortality rates.4-6,10,11 Studies show barriers to deprescribing include FRIDs the patient may be taking, their willingness to cooperate, their patient history, factors related to frailty, and the need for expertise in deprescribing medications due to possible adverse effects.5,11
The project used the define, measure, analyze, improve, control (DMAIC) model. The DMAIC model uses Six Sigma principles.18 This model is resourced and focused on achieving effective outcomes. Two studies utilized this model in falls prevention interventions with positive outcomes.18,19 The DMAIC model is also beneficial for compliance with the intervention. Kuwaiti and Subbarayalu state that nurse compliance with the intervention was 88%.19
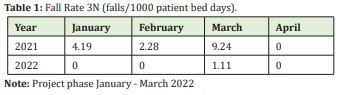
In the define phase, the QIC identified the problem through gap analysis. Information from the gap analysis is presented in Appendix A. Data collection plan development occurs during the measure phase. Table 1 shows the facility fall rate. The project team used Zoom meetings to discuss patient falls data during the analysis phase. During the improve phase, the QIC performed a root-cause analysis for the possible contributing factors highlighted in the analysis phase. In the control phase, a communication plan was created to monitor progress, discuss any possible issues, and make changes where necessary. The communication plan is shown in Appendix B.
This is a quality improvement that implemented the Medication Fall Risk Scale to reduce inpatient falls in the CSU. Project implementation took place in the CSU. The CSU is a five-bed unit accepting patients recovering from cardiovascular procedures. Inclusion criteria were patients of the CSU with scores of four or higher and prescribed two or more FRIDs. Exclusion criteria included patients of the CSU with fall risk scores lower than four (4<) and prescribed less than two (2<) FRIDs.
Intervention
Upon admission, staff assessed patients on:
- Medications (medication overuse, dose adjustment, IV access)
- Illness (stage, congestive heart failure, hypertension, comorbidities, dementia, prior fall history, diabetes, congestive heart failure, orthopedic surgery)
- Patient education (ability and willingness to learn)
- Lab results (international normalized ratio, therapeutic drug levels, electrolytes, hemoglobin/hematocrit) using the HDS and additional criteria from the MFRS.
The CSU charge nurse performed assessments using the MFRS. Patients with an MFRS score of six or greater received additional orthostatic blood pressure (OBP) monitoring. If there is a decrease of 20mmHG or greater in systolic and/or diastolic B.P., the attending physician must consult the pharmacist for medication recommendations. Patients meeting the criteria for additional monitoring (having MFRS score =/>6) received patient education, additional OBP monitoring, and continence management like toilet assistance and offering a bedpan. FRIDs included in the MFRS were specific to the setting and patient population.
During admission
Patient medication regimens were monitored in the Meditech system. Patient orthostatic B.P. data were collected in daily rounding (vital signs, pain scale, medication information). Patient-tailored prevention plans were used to prevent falls based on the recommendations from the pharmacist. Patient fall prevention plans for discharge were created based on patient needs and home setting. Meditech electronic medical records (EMR) system was used for record input, and IBM SPSS v.26 was used for data analysis.
This quality improvement intervention utilized the MFRS to reduce falls in the CSU. The number of recorded falls in the CSU during the intervention compared to pre intervention data was analyzed. Analysis of staff compliance during the intervention was also measured. Compliance was measured using the formula C/N(100). Where C equals the number of compliant charts, and N is the number of audited charts. Project oversight was not required. The Capella University Institutional Review Board determined the criteria for human research was not met by the project.
Design and instrumentation
The project uses pre- and post-intervention design (prior to and after implementing the MFRS). The project manager collected data using chart audits. The Medication Falls Risk Score (MFRS) tool and HDS assessed patient medication regimens on admission and determined their fall risk score. MFRS is part of the Fall Prevention Toolkit available from the Agency for Healthcare Research and Quality (AHRQ).2 The AHRQ implies permission because it is a public access website. Due to pandemic protocols, the CSU charge nurse performed the patient assessments using the MFRS tool. The project manager audited the maximum number of charts 5 each day. The project took place over 10-weeks. There were 50 charts audited. Of the 50 charts, 35 charts fit the criteria for patients with increased fall risk.
The Medication Fall Risk Score (MFRS) is the IRB approved tool used in the project Appendix B. Validity and reliability of the MFRS in a study using data from two hospitals. According to Yazdani & Hall,9 adding the MFRS tool improved screening sensitivity when compared using the Morse Fall Scale (MFS) alone. Scores using MFRS and MFS showed 66.65% specificity versus 61.37% using MFS without a loss in sensitivity.9
The hospital currently uses the Hester-Davis Scale (HDS) to assess for falls Appendix B. The HDS is utilized in many health care facilities as part of fall prevention protocols. Kientz & Hester validated the HDS in practice anticipating 13 falls of emergency department patients.20
Two falls were recorded during the duration of the project. Neither fall caused injury to the patient. Both falls were nurse-assisted. Comparing pre-intervention data with post-intervention, the MFRS helped prevent falls in the CSU. No patient medication regimens were changed during the intervention Appendix C.
Confounding Variables
The patients of the CSU were there for an average of one week. As a result, no medication regimens changed. Covid-19 protocols prevented the student from conducting patient assessments in person as only the CSU charge nurse was authorized to contact the patients in that unit. Non-drug-related fall risk factors were not available to the student.
Analysis
Patient demographic data and patient medication use were analyzed using descriptive statistics and frequencies. The descriptive statistics measured include the maximum, minimum, and mean. Descriptive statistics highlight patterns in project data. There were 50 charts audited. Of the 50 charts, 35 charts fit the criteria for patients with increased fall risk. Data included the week of intervention, patient demographics (age, gender, initials), fall risk score (FRS) upon admission, second day FRS, third day FRS, the number of medications prescribed, the number of falls risk inducing drugs prescribed, falls during their stay, and the categories of the medications included as FRIDs taken by the patients.
The project focused on by adding the MFRS to prevent patient falls in the CSU and staff compliance with project protocols. Patient falls are a leading cause of the increased length of stay in hospitals, increased health care costs, and patient injuries.4,14 However, inpatient falls are due to many different factors that are interconnected and complex. Falls risk-inducing drugs (FRIDs) are medications known to increase the risk of inpatient falls, such as antihypertensives, antipsychotics, diuretics, and opioids.5,7
Hospital records show the cardiac stepdown unit (CSU) experienced a 51% increase in patient falls and had the highest fall rate of any hospital unit with increased patient falls, and patient falls with injury. The CSU fall rate pre-intervention was 4.10 per 1000 bed stays. Post-intervention CSU fall rates reduced to 1.11 per 1000 bed stays (Table 1). The quality improvement coordinator performed a root-cause analysis and determined a deficit in current patient fall assessment criteria. Analysis of contributing factors by the QIC showed four possible contributing factors for high falls. Factors include the need for increased monitoring of high-risk patients; patient falls induced by medication, inadequate identification of high-risk patients, and lack of assistance for patients with bathroom. The project manager proposed improving patient assessment criteria. The goal was to create a routine that included monitoring FRIDs and orthostatic blood pressure.
Some limitations were inherent to the project. The sample size was very small, and it was conducted at one site. Results cannot be generalized beyond the practice site. The data analysis showed a prevalence of FRIDs prescriptions. Patient medication regimens were unchanged during admission. Medication regimens must be optimized before admission to the CSU. This is due to the short length of stay for CSU patients.
Descriptive statistics (mean, median, mode) were used to measure frequencies of FRIDs, recorded falls, fall risk scores, and falls during stay. Data analysis showed a prevalence of FRIDs prescriptions. Results indicate that the use of FRIDs is expected in the CSU. Patient medication regimens were unchanged during admission. Medication regimens must be optimized before admission to the CSU. Optimizing CSU medication regimens to decrease FRID is an important consideration when attempting to reduce falls.
A policy that reflects collaborative efforts is necessary at the local, state, and federal levels to continuously improve efforts for fall reduction in health care facilities. Health care professionals must collaborate with public health agencies to develop informed policies that support improvement initiatives. Such policies can facilitate understanding the effects of fall risk-inducing drugs and how to develop strategies for deprescribing using stakeholder insight as a guide.
The project site is implementing the intervention facility-wide. Intervention sustainment require policies that support team cohesion, communication, and employee retention.14,16 In this manner, the intervention is self-sustained and integrated into the current fall prevention strategy. The benefits reach all stakeholders as the organizational culture to support the initiatives facilitates patient safety, staff retention, and continuous improvement.
The project recorded two falls in its duration. Each fall was an assisted fall as a nurse was there to guide the patient to the floor.21 Both patients were exposed to polypharmacy, with one patient (male age 52) being prescribed six fall risk inducing drugs and one patient (female age 77) being prescribed 5 FRIDs. This is in accordance with research focused on fall prevention, polypharmacy, and elderly patients that shows polypharmacy is prevalent in the geriatric patient population.5-9 Both patients were assessed as high risk (MFRS score =/>6) and received orthostatic blood pressure monitoring. The patient medication regimen was not changed for either patient after physician review. Falls decreased in the cardiac stepdown unit during the project. The evidence suggests project protocols reduced patient falls as predicted.22,23
The CSU was chosen because it has the highest increase in falls out of all hospital units. Communication and collaboration were essential aspects of this intervention. The current pandemic requires protocols that limit interactions with patients and coworkers to reduce virus transmission. However, communication between the charge nurse and pharmacist was considered to improve staff morale and feelings of support, according to a meeting between the intervention team (J.F. personal communication, January 4, 2022).
Patient falls decreased during the project. Prior to the project, orthostatic blood pressures were not taken in the CSU. Patients were educated about their additional risks and were made aware of the changes in care regarding the project. Analysis of pre-intervention and post-intervention falls still needed to determine the effectiveness of the intervention.
This was a nurse-led intervention. Nursing observations uncovered the deficit in fall prevention strategy for the facility. Collaboration, communication, and respect between disciplines were vital to the project's implementation, progress, and effectiveness. Nurses benefit from education on recognizing high-risk patients. Nurse education on FRIDs and how to use the MFRS improves patient safety.
None.
None.
The authors have no disclosures or conflicts of interest.
- 1. Michalcova J, Vasut K, Airaksinen M, et al. Inclusion of medication-related fall risk in fall risk assessment tool in geriatric care units. BMC geriatrics. 2020;20(1):1–11.
- 2. Agency for Healthcare Research and Quality [AHRQ]. Preventing falls in hospitals: A toolkit for improving quality of care. AHRQ. 2022.
- 3. Preventing Falls in Hospitals. (2018).
- 4. Chang TI, Park H, Kim DW, et al. Polypharmacy, hospitalization, and mortality risk: A nationwide cohort study. Scientific Report. 2020;10(1):18964–18964.
- 5. Bromfield SG, Ngameni CA, Colantonio LD, et al. Blood Pressure, Antihypertensive Polypharmacy, Frailty, and Risk for Serious Fall Injuries Among Older Treated Adults With Hypertension. Hypertension. 2017;70(2):259–266.
- 6. Najafpour Z, Godarzi Z, Arab M, et al. Risk Factors for Falls in Hospital In-Patients: A Prospective Nested Case Control Study. Int J Health Policy Manag. 2019;8(5):300–306.
- 7. Omer HMRB, Hodson J, Pontefract SK, et al. Inpatient falls in older adults: A cohort study of antihypertensive prescribing pre-and post-fall. BMC Geriatrics. 2018;18(1):58.
- 8. Silva AKM, Costa DCMD, Reis AMM. Risk factors associated with in-hospital falls reported to the Patient Safety Commitee of a teaching hospital. Einstein (Sao Paulo). 2019;17(1):eAO4432.
- 9. Yazdani C, Hall S. Evaluation of the "medication fall risk score." American journal of health-system pharmacy: AJHP: official journal of the American Society of Health-System Pharmacists. 2017;74(1):e32–e39.
- 10. Farrell B, Thompson W, Black CD, et al. Health care providers' roles and responsibilities in management of polypharmacy: Results of a modified Delphi. Can Pharm J (Ott). 2018;151(6):395–407.
- 11. Lee J, Negm A, Peters R, et al. Deprescribing fall-risk increasing drugs (FRIDs) for the prevention of falls and fall-related complications: A systematic review and meta-analysis. BMJ Open. 2021;11(2):e035978.
- 12. Gettens S, Fulbrook P, Jessup M, et al. The patients' perspective of sustaining a fall in hospital: A qualitative study. J Clin Nurs. 2018;27(3-4):743–752.
- 13. Heng H, Jazayeri D, Shaw L, et al. Hospital falls prevention with patient education: a scoping review. BMC geriatrics. 2020;20(1):140.
- 14. Eckstrom E, Neal MB, Cotrell V, et al. An Interprofessional Approach to Reducing the Risk of Falls Through Enhanced Collaborative Practice. J Am Geriatr Soc. 2016;64(8):1701–1707.
- 15. Hakvoort L, Dikken J, van der Wel M, et al. Minimizing the knowledge-to-action gap; identification of interventions to change nurses' behavior regarding fall prevention, a mixed-method study. BMC Nursing. 2021;20(1):80–80.
- 16. Lasater K, Cotrell V, McKenzie G, et al. Collaborative Falls Prevention: Interprofessional Team Formation, Implementation, and Evaluation. J Contin Educ Nurs. 2016;47(12):545–550.
- 17. Ng BJ, Le Couteur DG, Hilmer SN. Deprescribing Benzodiazepines in Older Patients: Impact of Interventions Targeting Physicians, Pharmacists, and Patients. Drugs Aging. 2018;35(6):493–521.
- 18. Morgan L, Flynn L, Robertson E, et al. Intentional rounding: A staff‐led quality improvement intervention in the prevention of patient falls. Journal of Clinical Nursing. 2017;26(1-2):115–124.
- 19. Kuwaiti AA, Subbarayalu AV. Reducing patients' falls rate in an Academic Medical Center (AMC) using Six Sigma "DMAIC" approach. Int J Health Care Qual Assur. 2017;30(4):373–384.
- 20. Kientz S, Hester A. Predictive Model Development and Validation of the Emergency Hester Davis Scale© for Fall Risk Screening. Nursing: Research and Reviews. 2020;10:1–7.
- 21. Venema DM, Skinner AM, Nailon R, et al. In an observational study, patient and system factors were associated with unassisted and injurious falls in hospitals. BMC geriatrics. 2019;19(1):1–10.
- 22. Jambawo S. Transformational leadership and ethical leadership: their significance in the mental healthcare system. British Journal of Nursing. 2018;27(17):998–1001.
- 23. Kiegaldie D. Using education interventions in falls research: a framework for evidence-based education design. 2019.

