Meesmann corneal dystrophy syndrome is a genetic disorder of the eye that affects the cornea. This condition is characterized by the formation of small round cysts in all parts of the corneal layer, called the corneal epithelium. Meesmann corneal dystrophy syndrome is caused by a mutation in the KRT12 gene, which is located in the long arm of chromosome 17 as 17q21.2, or the KRT3 gene, which is located in the long arm of chromosome 12, as 12q13.13.
Keywords: Meesmann corneal dystrophy syndrome, Genetic mutation, KRT2 & KRT12 genes
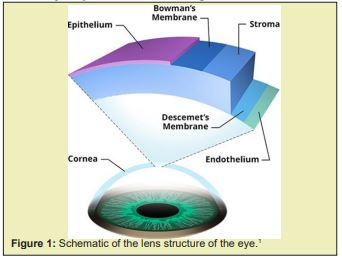
Meesmann corneal dystrophy syndrome is a genetic disorder of the eye that affects the cornea. This condition is characterized by the formation of small round cysts in all parts of the corneal layer, called the corneal epithelium. This part of the cornea acts as a barrier to prevent foreign matter such as dust and bacteria from entering the eye Figure 1.1
In people with Meesmann corneal dystrophy, cysts may appear very early in the first year of life. They usually affect both eyes and increase in number over time. Cysts usually do not cause any symptoms until late adolescence or adulthood, when they begin to rupture on the surface of the cornea and cause eye irritation. Potential symptoms usually include increased sensitivity to light (photophobia), abnormal blinking (blepharospasm), increased tear production, tenderness in the eye as if a foreign object has entered the eye, and inability to tolerate lens coverage. Some affected people also have a temporary dark area of vision Figure 2.1,2

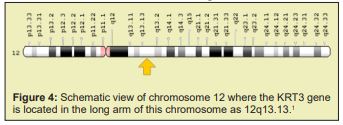
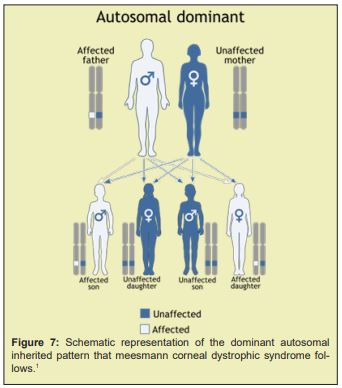
Meesmann corneal dystrophy syndrome is caused by a mutation in the KRT12 gene, which is located in the long arm of chromosome 17 as 17q21.2, or the KRT3 gene, which is located in the long arm of chromosome 12, as 12q13.13. These genes provide the instructions for the synthesis of proteins called creatine 12 and creatine 3, which are found in the corneal epithelium. The two proteins interact to form the structural framework of the corneal layer. Mutations in either the KRT12 or KRT3 genes weaken this framework, causing the corneal epithelium to become fragile and to develop cysts that characterize the disorder. Cysts may contain abnormal creatine protein masses and other cellular debris. When cysts rupture, they cause eye irritation and other symptoms of meesmann corneal dystrophy Figure 3.1,3 Meesmann corneal dystrophy syndrome follows an predominant autosomal inherited pattern. Therefore, a copy of the mutated KRT3 and KRT12 genes (either parent) is required to cause this syndrome, and the chance of having a child with this syndrome in an autosomal dominant state is 50%.1,4

Meesmann corneal dystrophy is a rare genetic disorder whose frequency of occurrence is unknown. The disorder initially affected a large family of several generations of Germans with more than 100 members. Since then, the syndrome has been reported in individuals and families around the world Figure 4.1,5
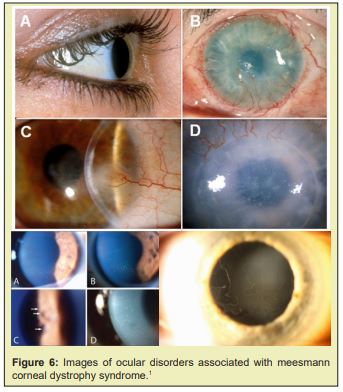
Meesmann corneal dystrophy syndrome can be diagnosed based on the clinical findings of some patients and some pathological and optological tests. The most accurate way to diagnose this syndrome is to do molecular genetic testing for the KRT3 and KRT12 genes to check for possible mutations Figure 5 and Figure 6.1,6

The treatment and management strategy of meesmann corneal dystrophy syndrome is symptomatic and supportive. Treatment may be performed with the efforts and coordination of a team of specialists, including an ophthalmologist and eye surgeon. There is no conventional treatment for this syndrome and all clinical measures are taken to alleviate the suffering of the patients. Genetic counseling is also essential for all parents who want a healthy baby Figure 7.1,7
In people with meesmann corneal dystrophy, cysts may appear very early in the first year of life. They usually affect both eyes and increase in number over time. Cysts usually do not cause any symptoms until late adolescence or adulthood, when they begin to rupture on the surface of the cornea and cause eye irritation. Treatment may be performed with the efforts and coordination of a team of specialists, including an ophthalmologist and eye surgeon.1-7
None.
None.
The authors declare no conflict of interest.
- 1. Asadi S, Pathology in medical genetics book. Amidi Publications. 2019;16.
- 2. Ehlers N, Hjortdal J, Nielsen K, et al. Phenotypic variability in Meesmann's dystrophy: clinical review of the literature and presentation of a family genetically identical to the original family. Acta Ophthalmol. 2008;86(1):40–44.
- 3. Irvine AD, Corden LD, Swensson O, et al. Mutations in cornea-specific keratin K3 or K12 genes cause Meesmann's corneal dystrophy. Nat Genet. 1997;16(2):184–187.
- 4. Klintworth GK. Corneal dystrophies. Orphanet J Rare Dis. 2009;4:7.
- 5. Nishida K, Honma Y, Dota A, et al. Isolation and chromosomal localization of a cornea-specific human keratin 12 gene and detection of four mutations in Meesmann corneal epithelial dystrophy. Am J Hum Genet. 1997;61(6):1268–1275.
- 6. Smith F. The molecular genetics of keratin disorders. Am J Clin Dermatol. 2003;4(5):347–364.
- 7. Szaflik JP, Ołdak M, Maksym RB, et al. Genetics of Meesmann corneal dystrophy: a novel mutation in the keratin 3 gene in an asymptomatic family suggests genotype-phenotype correlation. Mol Vis. 2008;14:1713–1718.

