Background:Dementia is a cognitive degenerative disease generally associated with Alzheimer disease, but victims with Parkinson’s disease also develops dementia at the latter stage. Dementia associates with irreversible loss of memory, and no medicinal cure is yet available. We here put some light on possible cell therapy for dementia.
Aim: Neural stem cells are multipotent cells which are capable of self-replication and differentiation into neurons, astrocytes or oligodendrocytes in the central nervous system. They produce Dopamine, neural factors, and therefore, one can expect that NSC transplantation can ultimately provide a better therapeutic approach in the treatment of dementia as well as Parkinson’s disease (PD).
Methods: We discussed the merits and demerits of using hNSCs cells over other possible candidate cells.
Results: As we found that hNSCs can secrete Dopamine as well as some neurotropic factors, like Brain-Derived Neurotropic Factor (BDNF) and Glial cell-Derived Neurotropic Factors (GDNF) which can support the proliferation of hNSCS and its Dopamine production ability, hNSCs can supply dopamine and also can stop α-synuclein aggregation.
Conclusion: hNSCs, therefore, could be a better cell regiment for cell transplantation therapy for dementia as well as PD.
Keywords
Dementia, Parkinson’s disease, Dopamine, Human neural cells (hNSCs), α-synuclein
Possible therapies for dementia in PD
Dementia is a broad term that stands for an irreversible loss of thinking ability, memory, and other mental capabilities. The cause is still unknown, but believed to be due to aging, loss of neural cells due to some neurotoxic agents, external brain injury, etc. However, Dementia/Alzheimer Disease is still considered as an idiopathic disease, like Parkinson’s Disease (PD).1,2
In fact, Dementia is not a disease, rather a group of symptoms caused by various conditions. Dementia generally associated with Alzheimer patient, but also found with PD, where the motor neuron defects, slow muscle movements, posture defects are the main classic symptoms.3 The scanty supply of Dopamine, a neurotransmitter, due to the loss of DA-ergic neural cells in the substantia nigra (SN), causes the development of PD4. The less availability of Dopamine in the Hippocampus region, the center of learning and memory in the brain, can also cause the damage of the brain cells there, and develops dementia.5
The key brain changes linked to Parkinson’s disease (PD) and Parkinson’s Disease Dementia (PDD) are abnormal microscopic deposits of alpha-synuclein, a protein found widely in the brain with a normal function not yet known. The deposits are called “Lewy bodies” after Frederick H. Lewy, M.D., the neurologist who discovered those in1900s. Lewy bodies are found in several other brain disorders, including Lewy body dementia (LBD). Evidence suggests that Lewy body dementia (LBD), Parkinson’s disease (PD) and Parkinson’s disease dementia (PDD) may be linked to the same underlying abnormalities in the brain processing of alpha-synuclein, which forms tangles and stop the cell-cell communication for neural transmission.6
About 5-8% of adults over age 65 have some form of dementia. This percentage doubles every 5 years after 65. As many as half of people in their 80s have some dementia, but may improve with treatment. However, many of the diseases that cause dementia aren't curable. Here we will discuss the possible therapeutic aspects of dementia.
Therapeutic Aspects
Experts don't yet understand how to prevent Parkinson's disease. In some instances, there seems to be a genetic predisposition to develop Parkinson's disease, but this isn’t always the case. Research is underway to find new ways to treat and prevent the disease. Treatment of dementia depends on its cause. In the case of most progressive dementias, including Alzheimer's disease, there is no cure and no treatment that slows or stops its progression. But there are drug treatments that may temporarily improve symptoms. The same medications used to treat Alzheimer's are among the drugs sometimes prescribed to help with symptoms of other types of dementias. Non-drug therapies can also alleviate some symptoms of dementia. Ultimately, the path to effective new treatments for dementia is through increased research funding and increased participation in clinical studies.
Drug therapy
Cholinesterase inhibitors: Cholinergic deficits are prominent in patients who have dementia associated with Parkinson's disease. In a double-blind, placebo-controlled study,7 showed that rivastigmine, an inhibitor of acetyl cholinesterase and butyryl-cholinesterase, led to meaningful treatment benefits in patients with dementia with Lewy bodies.7
Antipsychotic drugs: A drug category sometimes prescribed for behavioural symptoms of Alzheimer’s-should be used with extreme caution because they may cause serious side effects in up to 50% of those with Parkinson’s disease dementia or Lewy body dementia. Side effects may include sudden changes in consciousness, impaired swallowing, acute confusion, episodes of delusions or hallucinations, or appearance or worsening of Parkinson’s symptoms.
Carbidopa-Levodopa: Treating movement symptoms in those with Parkinson’s dementia can be challenging, because carbidopa- levodopa-the chief treatment for Parkinson’s movement symptoms- can sometimes aggravate hallucinations and confusion in those with Parkinson’s dementia or Lewy body dementia.
Anti-Depressant: Depression is common in individuals with Parkinson’s disease dementia and Lewy body dementia, and may be treated with a type of antidepressant called selective serotonin reuptake inhibitors (SSRIs). REM(rapid eye movement) disorder may be treated with clonazepam.
Surgery
Deep brain stimulation (DBS): A procedure called deep brain stimulation may also be used to treat Parkinson's disease. It sends electrical impulses into the brain to help control tremors and twitching movements. Some people may need surgery to manage Parkinson's disease symptoms. Surgery may involve destroying small areas of brain tissue responsible for the symptoms. However, these surgeries are rarely done since deep brain stimulation is now available.
Non-medicinal management of PD/AD/ Dementia
A routine exercise can help keep muscles flexibility and mobility. Exercise also releases natural brain chemicals that can improve emotional well-being.
- i. High protein meals can benefit your brain chemistry
- ii. Physical, occupational, and speech therapy can help your ability to care for yourself and communicate with others.
Cell therapy: The success of cell therapy depends on the right selection of cells
Among the above treatments nothing seems to be suitable for having a permanent cure from AD/PD/Dementia. However, the cure is possible if cell therapy can be done using a right cell that can grow, produce dopamine, can survive for longer period of times, but can differentiate, and should not have any ethical issues.
Human neural stem cells (hNSCs) can be considered as a potential therapeutic regiment to treat PD patients.8 hNSC contains Tyrosine hydroxylase (TH) that catalyzes the initial, rate-limiting step in the biosynthesis of catecholamines, including DA, noradrenaline, and adrenaline.9 The most important physiological aspect of functional hNSCs, as we see in our experiments, that they not only have the capability to synthesize DA but also release DA in response to substrate (DOPA)-induced condition than those obtained in control groups.10 These cells also express DAT (Dopamine Transporter), an another marker for mature and functional DA neurons, plays a key role in terminating dopaminergic signalling by catabolizing any excess DA which is neurotoxic also, to DOPAC,3,4-Dihydroxyphenylacetic acid.10
Therefore, hNSCs being equipped with DA production, release, and its breakdown, can efficiently control the physiologic level of DA in the synaptic cleft can be a better choice over any other.8 However, hNSCs is a slow growing cells and senesce after a few passages rendering a low level of supply for treatment. Attempts are going to develop in our lab a natural cell modification method by cell-cell interaction to increase the growth potential and survival length of hNSCs along with its DA-ergic quality.
Parkinson's disease is a movement disorder. It can cause the muscles to tighten and become rigid. This makes it hard to walk and do other daily activities. People with Parkinson’s disease also have tremors and may develop cognitive problems, including memory loss and dementia.
Parkinson's disease is most common in people who are older than 50. The average age at which it occurs is 60. But some younger people may also get Parkinson's disease. When it affects someone younger than age 50, it's called early-onset Parkinson's disease. Parkinson's disease is a chronic and progressive disease. It doesn't go away and continues to get worse over time. The absence of dopamine makes it hard for the brain to coordinate muscle movements. Low dopamine also contributes to mood and cognitive problems later in the course of the disease. Early onset Parkinson's disease is often inherited and is the result of certain gene defects. Parkinson's disease symptoms usually start out mild, and then progressively get much worse. The disease starts with: Tremors that affect the face and jaw, legs, arms, and hands; Slow, stiff walking; Trouble maintaining balance; Problems with coordination; and eventually get worse and include: Depression; Gastrointestinal problems (like constipation); Problems with urination; Trouble chewing and swallowing food; Memory loss; Hallucinations; Dementia; Weight loss.
Parkinson’s disease causes physical symptoms at first, and then gradually problems with cognitive function, including forgetfulness and trouble with concentration, may arise later. As the disease gets worse with time, many people develop dementia. This can cause profound memory loss and makes it hard to maintain relationships. Parkinson’s disease dementia can cause problems with: Speaking and communicating with others; Problem solving; Understanding abstract concepts; Forgetfulness; Paying attention, etc.
NSCs being equipped with DA synthesis and its breakdown to maintain the physiologic level of DA in the synaptic cleft can be a better choice over any other cells in these therapeutic lists, like induced pluripotent stem cells (IPSCs), Midbrain-derived hNSCs, and embryonic stem cells (ESCs). Propensity to form teratoma, ethical issues, and involvement of cumbersome processes are some from many to limit their uses clinically.11,12 hNSCs being a need-based supplier of DOPA will not produce any neural tube defects like long term DOPA therapy, and further these cells have DA scavenging systems, like Dopamine Transporter (DAT) and monoamino oxidase B enzyme.8 However, hNSC, since a slow growing cells and senesce after a few passages, it needs some modifications to increase their growth potential and survival length, along with their DA-ergic quality.
Cell-Cell interaction, a method for cell modifications was well known now-a-days and described elsewhere.13 We are presently attempting towards that strategy to improve the growth potential and survival length of hNSCs along with their capabilities to produce Dopamine and BDNF/GDNF. hNSCs, are equally active in synthesizing BDNF/GDNF proteins,14–16 which can prevent neuronal loss and induces regenerative response, during aging process with cognitive decline.14–22
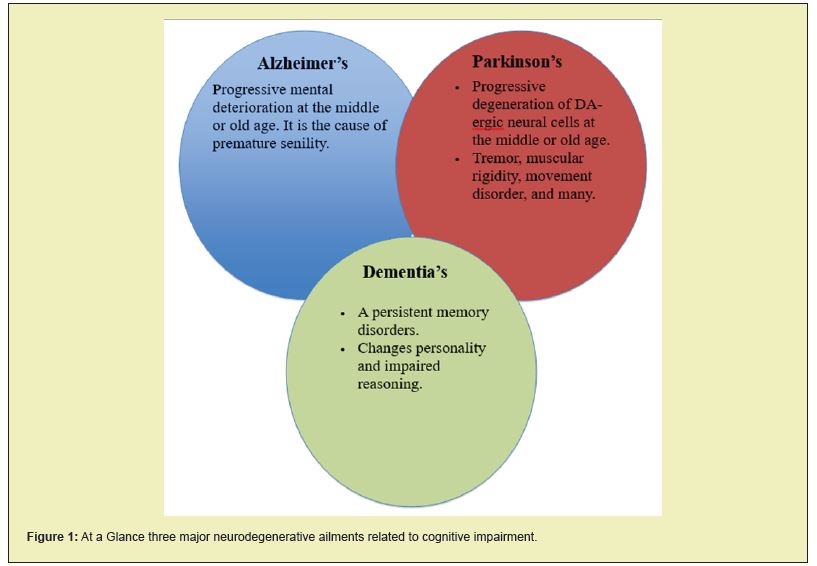
The conclusion of this paper is to show that hNSCs can be used for cell-therapy of Dementia as the disease is associated with scanty supply of Dopamine as well as deposition of alpha-synuclein (Lewy bodies) in the brain, which forms tangles and stop the cell-cell communication for neural transmission.6,23–25 In brief, a modified hNSCs in near future can be a solution for Dementia/AD/PD, the most yet unanswered neurodegenerative diseases. (Figure 1)
This research is supported by internal grant from AllExcel, Inc. Both the authors did contribute equally.
The authors report no conflicts of interest.
None.
- 1. Mayeux R, Chen J, Mirabello E, et al. An estimate of the incidence of dementia in idiopathic Parkinson’s disease. Neurology. 1990;40(10):1513–1517.
- 2. Ebmeier KP, Calder SA, Crawford JR, et al. Dementia in idiopathic Parkinson’s disease: prevalence and relationship with symptoms and signs of Parkinsonism. Psychological medicine. 1991;21(1):69–76.
- 3. National Parkinson’s Foundation: Parkinson’s and Dementia.
- 4. Alexander GE. Biology of Parkinson’s disease: Pathogenesis and pathophysiology of a multisystem neurodegenerative disorder. Dialogues Clin Neurosci. 2004;6(3):259–280.
- 5. Patel KP, Wymer DT, Bhatia VK, et al. Multimodality Imaging of Dementia: Clinical Importance and Role of Integrated Anatomic and Molecular Imaging. Radio Graphics. 2020;40(1):200–222.
- 6. Vasili E, Dominguez Meijide A, Outeiro TF. Spreading of α-Synuclein and Tau: A Systematic Comparison of the Mechanisms Involved. Mol Neurosci. 2019;12:107–130.
- 7. Emre M, Aarsland D, Albanese A, et. al. Rivastigmine for Dementia Associated with Parkinson’s Disease. N Engl J Med. 2004,351:2509– 2518.
- 8. Chakraborty A, Diwan A. Selection of Cells for Parkinson’s Disease Cell- Therapy. Int J Stem Cell Res Ther. 2019;6(1):063.
- 9. Colette Daubner S, Le T, Wang S. Tyrosine hydroxylase and regulation of dopamine synthesis. Arch Biochem Biophys. 2011;508(1):1–12.
- 10. German CL, Baladi MG, McFadden LM, et al. Regulation of the dopamine and vesicular monoamine transporters: Pharmacological targets and implications for disease. Pharmacol Rev. 2015;67(4):1005–1024.
- 11. Andersson EK, Irvin DK, Ahlsio J, et al. Ngn2 and nurr1 act in synergy to induce midbrain dopaminergic neurons from expanded neural stem and progenitor cells. Exp Cell Res. 2007;313(6):1172–1180.
- 12. Medvedev SP, Shevchenko AI, Zakian SM. Induced pluripotent stem cells: Problems and advantages when applying them in regenerative medicine. Acta Naturae. 2010;2(2):18–28.
- 13. Chakraborty AK, Diwan A. Cell-Cell Interaction A Method to Upgrade the Neural Cells Function. Journal of Neurology & Neurophysiology. 2020;11(4):001–003.
- 14. Skaper SD. The neurotrophin family of neurotrophic factors: an overview. Methods Mol Biol. 2012;846:1–12.
- 15. Huang EJ, Reichardt LF. Neurotrophins: roles in neuronal development and function. Annu Rev Neurosci. 2001;24:677–736.
- 16. Budni J, Bellettini-Santos T, Mina F, et al. The involvement of BDNF, NGF and GDNF in aging and Alzheimer’s disease. Aging and Disease. 2016;6(5):331–341.
- 17. Akerud P, Canals JM, Snyder EY, et al. Neuroprotection through delivery of glial cell line-derived neurotrophic factor by neural stem cells in a mouse model of Parkinson’s disease. J Neurosci. 2001;21(20):8108–8118.
- 18. Bishop NA, Lu T, Yankner BA. Neural mechanisms of ageing and cognitive decline. Nature. 2010;464(7288):529–535.
- 19. Baquer NZ, Taha A, Kumar P, et al. A metabolic and functional overview of brain aging linked to neurological disorders. Biogerontology. 2009;10(4):377–413.
- 20. Samanez-Larkin GR, Knutson B. Decision making in the ageing brain: changes in affective and motivational circuits. Nat Rev Neurosci. 2015;16(5):278–289.
- 21. Gill SS, Patel NK, Hotton GR, et al. Direct brain infusion of glial cell line-derived neurotrophic factor in Parkinson disease. Nat Med. 2003;9(5):589–595.
- 22. Ghribi O, Herman MM, Forbes MS, et al. GDNF protects against aluminum-induced apoptosis in rabbits by upregulating Bcl-2 and Bcl-XL and inhibiting mitochondrial Bax translocation. Neurobiol Dis. 2001;8(5):764–773.
- 23. Vasic V, Barth K, Schmidt MHH. Neurodegeneration and Neuro- Regeneration-Alzheimer’s Disease and Stem Cell Therapy Int J Mol Sci. 2019;20(17):4272.
- 24. Willis CM, Nicaise AM, Peruzzotti-Jametti L, et al. The neural stem cell secretome and its role in brain repair. Brain Research. 2020;1729:146615.
- 25. Sugaya K. Neuroreplacement therapy and stem cell biology under disease conditions. Cell Mol Life Sci. 2003;60(9):1891–902.

