Background: Urinary incontinence affects about 45% of all women, and stress urinary incontinence accounts for about 40%. Many women opt for surgical treatment when conservative management fails. One of the surgical treatments is bulking, that refers to a minor transurethral procedure where a bulking agent is injected into the submucosa of the urethra. Infected pubic symphysitis is an infection of the pubic symphysis that causes subpubic pain, disability and ultimately immobility. It is known to be a rare complication to urogenital procedures but has never been described after a bulking injection.
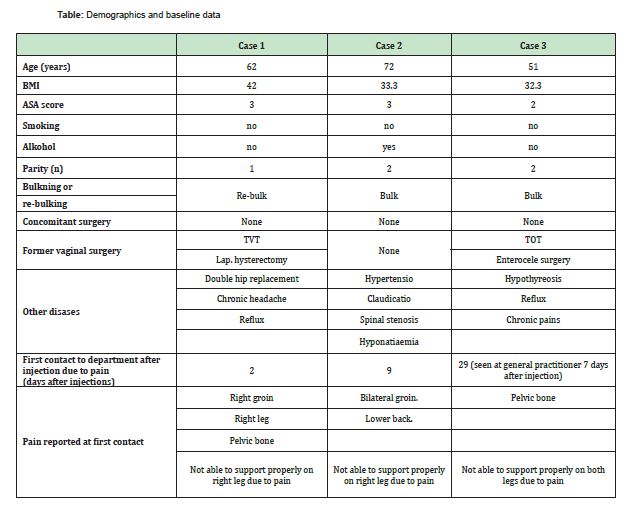
Case Report: We present three women with a story of infected pubic symphysitis after bulking injections. They all experienced pain within the first week after the injections. They all had pubic bone or groin pain and were not able to support properly on both legs due to pain. White blood cell counts and C-reactive protein were elevated, and Magnetic resonance imaging or computerized tomography scan showed signs of symphysitis. All women were treated with long term antibiotics and seen by or discussed with the orthopedic surgeons.
Conclusion: This review reports on a serious outcome, symphysitis, even after a minor surgical treatment. In our cases no fatality was observed, but two of the women still have chronic pain more than one year after the bulking injections. Due to these three cases, the standard procedure has now changed, and a pre-treatment of antibiotics is given to all women undergoing the bulking procedure.
Keywords: Urinary incontinence, Stress, Osteomyelitis, Pubic bone, Mobility limitation
Urinary incontinence (UI) is a condition that affects about 45% of the women above the age of 18 and increases with age.1 There are different types of UI, defined by the mechanism behind the UI. Stress urinary incontinence (SUI), accounting for about 40% of the UI cases,2 is defined as involuntary loss of urine on effort or physical exertion or on sneezing or coughing.3
For all types of UI, first line treatment is conservative. In the case of SUI, many women opt for surgical treatment when first-line conservative management fails.4 One of the surgical treatments for SUI is periurethral bulking. It is a minor procedure where a bulking agent is injected into the submucosa of the urethra to ensure coaptation.2
When the bulking procedure is performed at our department, it is done as an out-patient procedure. It is performed under local anesthesia with two ampullas of Citanest Dental Octapressin, injected periurethral, at 3 and 6 o’clock, one ampulla on each side. The expected risks are hematuria and cystitis. No antibiotics was given peri or postoperatively.
Infectious osteitis pubis or infected pubic symphysitis (IPS), a bacterial infection of the symphysis pubis, is a rare condition that ultimately causes disability, hospitalization and may require emergent therapy.5 Risk factors are urological surgery, being an athlete, pelvic malignancies, and intravenous drug use.6
We present three women with a story of symptoms of IPS after injection of a bulking agent. The cases were reported during the period from June 2021 to January 2023.
Case 1
A 62-year-old woman Table. A retropubic sling surgery was performed 16 years earlier. Due to recurrence of SUI, injection with a bulking agent was performed with success two years earlier but the incontinence reoccurred. She opted for treatment with re-injection with a bulking agent.
Two days after the re-injections, she was referred by her general practitioner (GP). She had a medical history of 24 hours of pain, located to her lower back, pelvic bone and right leg. Pain made standing on right leg impossible. She had no fever. Due to pain, she was hospitalized.
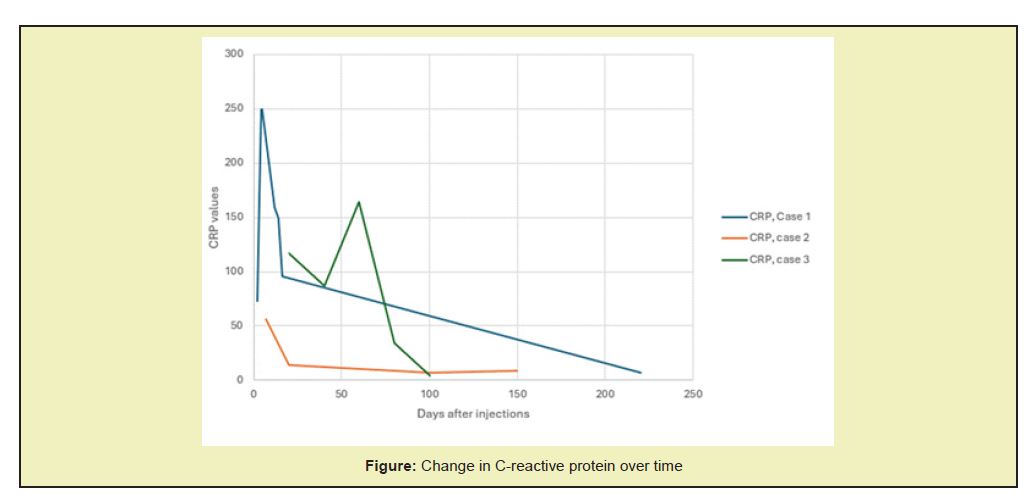
The day after admission her C-Reactive Protein (CRP) increased Figure and she developed fever (38.4 degree Celsius), which despite the treatment with intravenous (iv) Metronidazole 1 gram (g) twice a day (2/day) and iv Cefuroxime 1,5 g 3/day, increased to 40.5 degrees Celsius. Intravenous Gentamicin 403 milligram (mg), single dose, was added. On day eight after the injections, a positron emission tomography scan (PET-CT) was carried out. Her antibiotics was changed to a combination of iv Piperacillin and Tazobactam 1g 4/day and iv Vancomycin 2g 2/day. On the 13th day a magnetic resonance imaging (MRI) scan confirmed osteomyelitis (subchondral scleroses, infiltration of the soft parts). The treatment was changed to tablet Clindamycin 300mg 3/day for 6 weeks. Eight months after re-injection a control MRI was done. It showed sequelas after IPS, but no signs of active infection. A month later (nine months after re-injection) another MRI was done. It showed oedema, and a six-week treatment with tablet Dicloxacillin 1g 3/day was prescribed.
Ten months after the re-injection she still had pain but was doing better. Her blood test had all normalized and she was no longer in contact with the clinic. The orthopedic department was involved in diagnosis and treatment.
Case 2
A 72-year-old woman Table Diagnosed with mixed urinary incontinence. Her UUI was treated with medication (beta 3-adrenoceptor agonist and antimuscarinic agents), but unsuccessful. She signed up for Botox treatment. For her SUI, she opted for injection with a bulking agent.
Postoperatively contact was taken ten days after surgery due to suspicion of post operative residual urine (POUR). A story of bladder pain and pelvic bone pain was presented. No POUR was found. Contact was made again 12 days later (22 days after injection). Pain was localized as earlier but had increased in intensity. On examination a hematoma with the size of app. 1cm was found close to the pelvic bone. No fever but slight elevated CRP. Antibiotics, tablet Cefuroxime 500 milligrams (mg) 2/day for 14 days was prescribed. An MRI was ordered, but the woman canceled it.
One month after the injection the department was contacted again. The pain had increased, and active use of legs was difficult due to pain. The CRP count had increased. The leg pain disappeared spontaneously, but pain around the pelvic bone continued. Pain increased and contact was taken again 46 days after injections. Antibiotics (tablet Clindamycin 300mg, 3/day, for 6 weeks) was prescribed, and status was followed with blood samples for a month. An MRI done 90 days after injections described extreme oedema around the pelvic bone and infiltration of the soft parts compatible with IPS. Contact was taken to the orthopedics department. Here a decision not to take more action was taken due to normalized clinic and blood test.
Due to other health issues a PET-CT was done five months later the same year. This still showed changes described as symfysitis. Clinical there were no signs of IPS, and no further action was taken.
Eight months after the injections, all pain was gone.
Case 3
A 51-year-old woman Table presented due to relapse of SUI after surgery with a trans-obturator sling 16 years earlier. Opted for injection treatment with a bulking agent.
She attended the gynecological emergency department one month after treatment with bulking injections. She presented a history of pain starting two days after the injections. She had been seen by her GP one week after the injections. CRP had been marginally increased, but when she was seen by her GP again two weeks later it had increased further, and tablet Ampicillin 1g 4/day for 7 days was prescribed on suspicion of urinary tract infection (UTI). When this did not help, she was admitted to the gynecological emergency room. At the hospital her CRP was normal, and she presented with no fever. She had pain despite the use of painkillers.
A week later a PET-CT scan was carried out. It showed potential inflammation around the pubic bone. Hence a treatment with tablet clindamycin 300mg 3/day was given, intentionally for three months. Contact was kept. Pain was unchanged after another two months treatment (3 months after injection) and she was referred to the orthopedic department. An MRI scan confirmed the diagnose IPS (subchondral scleroses, erosion and edema of the pubic bone, infiltration of the soft parts). Surgery was suggested, but since her infection numbers had lowered Figure conservative treatment was chosen. During the next year, symptoms varied from better to worse and back, and periodically a small rise in CRP was observed. She received a treatment of antibiotics again (tablet Amoxic/Clavulanate 500+125mg 3/day for 6 weeks) almost a year after the injections, and after this there has been some improvement of her pain. She is however, not back to her normal performance.
No literature on IPS after injection with a bulking agent was found. However, IPS is described as a condition seen in relation to larger and more invasive incontinence surgery such as the Burch procedure7 and after laparoscopic retropubic sling procedure.8 Female incontinence surgery is found to account for about 24% of the IPS cases.6
The Typical features of IPS are described to included fever (74%), pubic pain (68%), painful or waddling gait (59%), pain with hip motion (45%), and groin pain (41%).6,7,9,10 These symptoms were found among all three of our cases. A differential diagnosis is osteitis pubis, a non-infectious inflammation of the pubic symphysis.
Diagnosis is based on clinic supported by microbiologic culture results, image methods, and proteins augment during acute phase.9,10 In the literature on IPS, radiographs are described to show disjunction of the pubic bone with irregular shoreline.10 Both computerized tomography scan (CT scan) and MRI can show erosions of the banks of the pubic symphysis with infiltration of the soft parts.9,10 All the cases described had both an MRI and a PET-CT done describing infiltration of the soft parts and erosions of the pubic bone.
Only one of the women described (case 1) had a fever. Case 1 is also presenting with the most elevated CRP Figure 1 and the only one treated with intravenous antibiotics. Case 2 never presents with a high increase in CRP. Her compliance is low, and it is not possible to follow her as closely as the other cases. Case 3 has shortly an increase in infection numbers, but then normalizes initially. She does however later have small increases in CRP and is treated with antibiotics. Case 2 and 3 are however the ones with the most severe changes on MRI.
In the cases described no growth of bacteria was found. No biopsies were taken from the pubic bone. Only microbiologic culture from blood, urine and vaginal swaps were taken, and they were all without growth. In the literature growth of bacteria is most often isolated by biopsy of soft tissue7,8,10 and seldom from vaginal swabs.10 Patients with recent urinary incontinence surgery are usually found to have a monomicrobial infection, with no predominant pathogen. One study evaluating 24 women with IPS after incontinence surgery found thar Staph. aureus was seen in 5(21%), P. aeruginosa in 4(17%), Escherichia coli in 4(17%), polymicrobial infection in 4(17%), Enterococcus species in 3(13%), and miscellaneous organisms in 5(21%).6
For treatment of IPS an antibiotic course of 6 weeks' duration is recommended, and a surgical debridement is required in 55% of patients6 Since the three cases of IPS, the procedure for injections with a bulking agent has been changed at our department. After a dialogue with the orthopedic surgeon, all women are given a single dose of 1g Cefuroxime orally one hour before the injection procedure.
None.
This Case Report received no external funding.
Regarding the publication of this article, the authors declare that they have no conflict of interest.
- 1. Schreiber Pedersen L, Lose G, Høybye MT, et al. Prevalence of urinary incontinence among women and analysis of potential risk factors in Germany and Denmark. Acta Obstet Gynecol Scand. 2017;96(8):939-948.
- 2. Sandvik H, Hunskaar S, Vanvik A, et al. Diagnostic classification of female urinary incontinence: an epidemiological survey corrected for validity. J Clin Epidemiol. 1995;48(3):339-343.
- 3. Haylen BT, de Ridder D, Freeman RM, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Int Urogynecol J. 2010;21(1):5-26.
- 4. AUGS-IUGA Joint Publication. Joint report on the terminology for surgical procedures to treat stress urinary incontinence in women. Developed by the Joint Writing Group of the American Urogynecologic Society and the International Urogynecological Association. International Urogynecology Journal. 2020;31:465-478.
- 5. Devlieger B, Wagner D, Hopf J, et al. Surgical debridement of infected pubic symphysitis supports optimal outcome. Arch Orthop Trauma Surg. 2021;141(11):1835-1843.
- 6. Ross JJ, Hu LT. Septic arthritis of the pubic symphysis: review of 100 cases. Medicine (Baltimore). 2003;82(5):340-345.
- 7. Michiels E, Knockaert DC, Vanneste SB. Infectious osteitis pubis. Neth J Med. 1990;36(5-6):297-300.
- 8. Kroft J, Kung RC. Postoperative pubic symphysis osteomyelitis after laparoscopic two-team sling with anterior and posterior colporrhaphy. J Minim Invasive Gynecol. 2009;16(4):513-515.
- 9. El Mezouar I, Abourazzak FZ, Mansouri S, et al. Septic arthritis of the pubic symphysis: a case report. Pan Afr Med J. 2014;18:149.
- 10. Alaya Z, Zaghouani H, Osman W, et al. Septic arthritis of the pubis symphysis: clinical and therapeutic features. Pan Afr Med J. 2017;26:215.

