Introduction: Papillophlebitis is a rare condition that may present clinically like an incomplete central retinal vein occlusion (CRVO). Papillophlebitis is a rare ocular condition that typically affects young (20-35 years old), previously healthy patient. Papillophlebitis can lead to ischemic CRVO with resulting macular edema and poor visual outcome.
Aim: Aim of our case report is to present a rare case of a young male patient with papillophlebitis and to present the treatment that we gave to the patient with a good result.
Case report: Patient, A.L., male, born 1986, came to our Clinic with sudden loss of vision on the right eye. First he had dark shadow in the right eye 15 days before he lost vision on the right eye. He was diagnosed with arterial hypertension. He does not have any previous medical history, but he had injury of the right eye 1993, he did not have surgery only local therapy and without any consequences. VOD: sc 2/60, VOS: sc 1.0, TOD: 16 mmHg, TOS: 17 mmHg. Slit lamp examination showed on the right fundus optic disc edema, retinal venous dilation and tortuousity, and intraretinal hemorrhages around optic disc and macula. Optical coherence tomography showed macular edema. Laboratory testing showed high concentration of coagulation factors: II,V, VII, IX, X, XII, and protein C. Immunology testing were negative. We treated him with high doses of intravenous methylprednisolone and we gave intravitreal bevacizumab in the right eye. He was discharged with significantly improved vision and local status on the right eye was better.
Conclusion: We consider that the inflammatory reaction and reaction and the coagulation alternation present risk factors for the development of papillophlebitis. Also, we suggest that anti-VEGFs, with corticosteroids, are beneficial for treating papillophlebitis when visual acuity is decreased due to subretinal fluid.
Keywords: Papillophlebits, Optical coherence tomography, Methylprednisolone
Papillophlebitis is a rare disease and in some reports considers as a clinical variant of central retinal vein occlusion (CRVO) that is typically seen in healthy young adults.1 Risk factor for papillophlebitis are: hypercoagulable state, thrombophilia, vasculitic syndromes, blood hyperviscosity, and other recognized systemic vascular inflammatory disorders.2 Visual symptom is painless unilateral visual acuity (VA) unlike typical CRVO, patients with papillophlebitis usually present with normal or near normal VA, and visual final prognosis is more favorable.3 But also papillophlebitis can lead to ischemic CRVO with resulting macular edema and poor visual outcome.4 The differential diagnosis of papillophlebitis includes CRVO, nonarteritic ischemic optic neuropathy, diabetic papillopathy, infectious papillitis, hypertensive retinopathy, prethrombotic retinal vein, and orbital compressive lesions. An evaluation for hypercoagulable disorders must be considered.
Usually the clinical course of papillophlebitis is typically without permanent visual loss, and spontaneous improvement is common. Up to 30% of patients with papillophlebitis develop ischemic venous occlusion and could develop neovascular glaucoma; and some will have macular edema leading to poor visual acuity. Decreased VA secondary to macular edema or areas of ischemia and neovascularization are an indication to establish treatment. If they are not diagnosed and treated immediately, papillophlebitis may will have a poor prognosis.1
A 42-year-old man came to our Clinic with sudden vision loss on the right eye. He said that first he saw dark shadow on the right eye 15 days ago and now that he got sudden loss of vision. He had injury of the right eye 1993, he did not have surgery only local therapy and without any consequences. He was diagnosed recently with arterial hypertension and got the medication. No relative afferent pupillary defect (RAPD) was detected. VOD: sc 4/50, VOS: sc 1.0. Ophthalmoscopy showed optic disc edema, retinal venous dilation and tortuousity, and intraretinal hemorrhages around optic disc and macula, and cotton wool spots. Optical coherence tomography showed macular edema Figure 1.
From his blood we took laboratory testing factor of coagulation, which showed high concentration of coagulation factors: II,V, VII, IX, X, XII, and protein C. Immunology testing were negative.
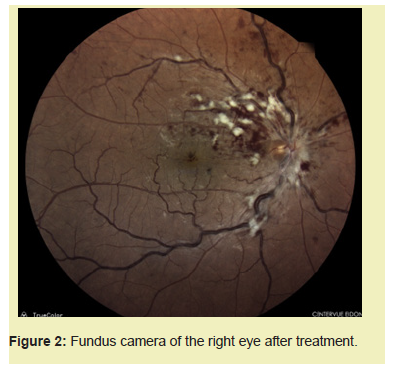
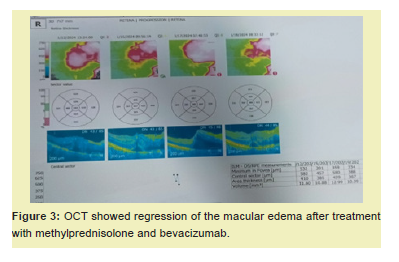
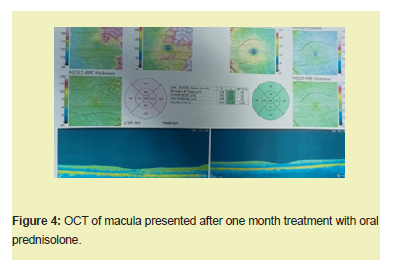
The patient was initially treated with high-dose methylprednisolone (1g/day) for five days and after continued with oral prednisolone for a month with reduction of a dose. On the Clinic we gave him bevacizumab intravitreal in the right eye and also, we gave anticoagulation therapy and therapy for hypertension. He was discharged with visson improvement, VOD: sc 0.8-0.9, and also with reduction of macular edema and ophthalmoscopy showed regression optic disc edema, less intraretinal hemorrhages and cotton wool exudates Figures 2-5.


Papillophlebitis is a rare condition that may present clinically like an incomplete central retinal vein occlusion (CRVO).5 Papillophlebitis is a rare ocular condition that typically affects young (20-35 years old), previously healthy women, but also men. Papillophlebitis is often misdiagnosed as papillitis or papilledema.6 The presence of retinal venous dilation and tortuosity, vitreopapillary traction, and scattered intraretinal hemorrhages should suggest secondary rather than primary optic disc edema. Testing with OCT or fluorescein angiography may help in differentiating PP from CRVO. Many authors believe papillophlebitis is a form of inflammatory CRVO and although the prognosis is generally favorable, papillophlebitis can lead to ischemic CRVO with resulting macular edema and poor visual outcome.7 Significant macular edema with decreased VA is an indication to initiate treatment in order to avoid irreversible macular damage.1 Corticosteroids are the conventional treatment for papillophlebitis.8 Furthermore, anti-vascular endothelial growth factor (VEGF) has been used to treat the ME of CRVO.7
Since spontaneous recovery from papillophlebitis is also very common, treatment should be considered only when there is the possibility of macular damage, which would reduce VA. In the case presented here, we administered intravitreal bevacizumab in the right eye, intravenous methylprednisolone, 1g for five day, with one month therapy with oral prednisolone. We had better results in visual acuity and also macular edema regression.
Comparing to our case report, in the case report of İnci Güngör et al the patient was young, with no defined risk factor for retinal ischaemia. Initial VA was normal, the peripapillary distribution of retinal exudates gave the impression of papillophlebitis, not CRVO. Based on the appearance of the retina, their final diagnosis was papillophlebitis. They administered intravitreal ranibizumab together with conventional treatments, including oral steroids and antibiotics, since papillophlebitis is considered by some to be a subtype of CRVO.2 Their patient showed a rapid improvement in VA, with resolution of the subretinal fluid within 2 weeks post-injection, also as per patient.
We suggest that anti-VEGFs, also with corticosteroids, are beneficial for treating papillophlebitis when VA is decreased due to subretinal fluid. Based on the similarity of their clinical aspects and origins, we reasoned that application of intravitreal anti-vegf, which is effective in treating CRVO, would be beneficial in treating papillophlebitis.7
We consider that although intravitreal anti-VEGFs injections are not a routinely recommended treatment for papillophlebitis, it should be considered as a potential therapeutic option in selected cases as is our case.
None.
This Case Report received no external funding.
Regarding the publication of this article, the authors declare that they have no conflict of interest.

