Background: Mandibular prognathism in Class 3 malocclusion (CLIII) is one of the most severe maxillofacial deformities. Fortunately, most of this malocclusion cases can be treated by facial growth modification, using extra and/or intra-oral appliances in growing individuals. Occipital-pull chin cup is the extra-oral orthopaedic appliance, which was mostly used for the treatment of mandibular prognathism in growing Class 3 1(Ngan, Sung, 2015). Unjustifiably, most orthodontists I know do not use chin cup therapy in the treatment of CLIII. Therefore, being new to the field of orthodontics, I needed to build a highly evidenced based knowledge on chin cup therapy’s effectiveness in the treatment of developing CLIII with prognathic mandible.
Objective: Through a narrative literature review, the aim of the study was assessed following scientific methodology. Articles published from January 2010- November 2020 (commencement of the current review) were collected using keywords derived from PICO. Only highly evidence based studies (randomised and non-randomised clinical trials) with the least risk of bias scores were selected, and critically appraised using the Critical Appraisal Skill Programme (CASP). Results were used to draw the conclusion.
Material and Method: The study title was broken down into its PICO (population, intervention, comparative, outcome) components and search keywords were derived. These were used to carry out a literature search through electronic search engines (Medline-PUBMED, Science Direct, ISI Web of Knowledge, Research gate, Google Scholar, Cochrane library and hand searching of references list. Collected articles were assessed for risk of bias using Downs and Black (D&B) scale. Papers with score ‘good’ and above’ on the D&B assessment were critically appraised. PRISMA statement reporting format and Harvard referencing system were adopted in the study.
Result: Following the Downs and Black assessment only 4 studies were found at a level worthy to be critically appraised. Results of all the four articles revealed that chin cup therapy produced significant growth modification in the mandible, when applied at an early age. Moreover, chin cup was also found to increase the lower anterior facial height significantly. All the papers considered only the short-term effect of chin cup, but not the long-term effect. Treatment results stability was also not reported.
Conclusion: The significant improvement in CLIII manifestation in the selected articles, make it possible to conclude that chin cup is viable for the treatment of CLIII malocclusion with mandibular prognatism. However, treatment results stability needs to be researched.
Keywords: Class 3 malocclusion (CLIII), Maxillofacial deformities, CASP
Abbreviations: CLIII: Class 3 malocclusion; PICO: Population, Intervention, Comparative, Outcome of the study; CASP: Critical Appraisal Skill Programme; D&B: Downs and Black risk of bias assessment tool; PRISMA: Preferred Reporting Items for Systematic Reviews and Meta-Analyses, CC: Chin Cup; CD-ROM- Compacy Disc; MD955: Dentistry Professional Project; PM: Prognathic Mandible; AOBP: Acrylic occlusal bite plane (on lower posterior to open the bite anteriorly); Tx: Treatment; Yrs: Years; SPSS: Statistical analysis of variables using software package, ANOVA: One way Analysis of Variance; TPS: Thin plate spline (deformation grid).
Occipital-pull chin cup is the extra-oral orthopedic appliance mostly used for the treatment of mandibular prognathism in growing Class 3 malocclusion.1,2 This appliance is available in several models and designs, but they are all generally composed of a plastic, acrylic, or rubber chin cup attached to elastic bands that fit over the crown of the head. The bands apply adjustable force on the mandible to limit its growth, hence allow the upper jaw to outpace the mandibular growth. This process aids in achieving a more harmonious facial profile in patients with Class 3 malocclusion. Chin cup, can be worn twelve or more hours per day for several months to some years.3
Mandibular growth restraining devices that resembled the contemporary chin-cup were reported in 1800s.4,5 However, those tended to be inefficient for mostly three reasons:
- The forces applied by the devices were not strong enough to influence the condylar growth
- Treatment mostly started after the condylar growth maturation
- Clinicians had limited knowledge of growth guidance.5
The unsatisfactory results of the chin-cup therapy, led orthodontists at that time to the use of inter-maxillary elastics, to camouflage the skeletal CL III malocclusion by dento-alveolar correction. Despite that, most of the masking outcomes were compromised and unsatisfactory. In 1940’s and early 1950’s the evolution of Milwaukee brace treatment that remarkably altered growth and shape of the mandible, encouraged clinicians to return to orthopedic approach in attempts to treat Class III skeletally rather than dental-alveolar corrections only.
Graber (1977) in a research claimed the following:
- High ‘orthopedic’ forces (400 to 800g) might improve mandibular prognathism.
- The ‘orthopedic force’ in chin cup therapy works by directing sufficient forces to the mandibular basal bone through a chin cup device.
- The design of chin cup did not change significantly, but the force applied by the device was increased and that improved the effectiveness of the device remarkably.
- Results of clinical studies were variable due to differences in appliance design, force application, and evaluation technique. Studies that reported failure had used the therapy on primarily teenage patients and applied light chin cup forces.
- Studies that reported success emphasized the importance of early age intervention of chin cup, using stronger orthopedic force.
- Chin cup growth modification “has been a subject for much opinion but little research.”
Until the present time, chin cup therapy remains a controversial topic among researchers and clinicians. Not only because of the different opinions on the magnitude of force to be applied, but also due to:
- The absence of a standard protocol for the efficient and proper use of chin-cup;
- The effectiveness of the device in studies is contradicting.6 Numerous authors including Profitt 2000, Bishara 2001, and Chang 2005, supported chin cup effectiveness, while, Mc Namara 2005, Sugaura 2005, Oppenheim 1944, Thilander 1965, doubted it;
- Insufficient investigation about the effect of chin cup therapy on facial soft tissues.7
- Most of the relevant studies conduct a short-term follow-up period,7 therefore, the long-term effect of chin-cup therapy continues to be questionable.8,9
- Lack of investigation on the compliance of the candidates wearing chin-cup devices.
- Limited researches comparing other modalities to chin-cup therapy, in treatment of CLIII malocclusion.
Despite this long list of potential uncertainties I would like to initially only focus on the effectiveness of the therapy in correcting Class 3 malocclusion using this preliminary study. If it does show promising results I would likely progress this study into a second part to explore the remainder items. I will report on any findings that I do come across but I have not added these to my aims due to time and resource constraints of this study.
Objectives: the aim will be assessed through a narrative literature review of previous relevant studies, published in online journals from January 2010- November 2020. Only highly evidence based studies (randomised clinical trials, and Cohort studies) are to be included. During the search process specific keywords were used initially to collect data, then final selection relied on the following:
- Inclusion and exclusion criteria
- Duplicates removal
- Full text availability
- Downs and Black checklist to be used to exclude biased studies
- CASP tool for final critical appraisal
confirmatory narrative literature review (Protocol for this article exists)
A narrative literature review is likely the best approach to fulfill the aim study, as it makes new discoveries possible due to the less restricted methodology.
Study Characteristics
Study design: English confirmatory narrative literature review of previous randomized and non-randomized controlled trials
Study framework: (PICO)
Population- patients with developing Class III due to prognathic mandible
Intervention- chin -cup (CC) therapy
Comparator- No treatment
Outcomes- Successful treatment of CLIII (mandibular prognathism)
S: Narrative literature review
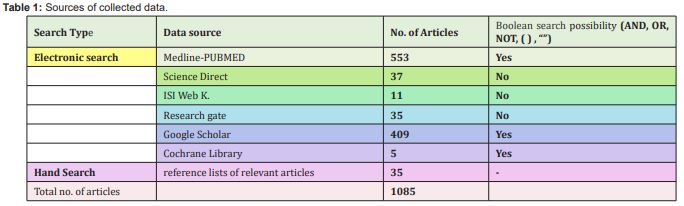
Sources of Data Collection (summary displayed in Table 1)
A) The electronic database search include:
-Medline-PUBMED
-Science Direct,
-ISI Web of Knowledge search engines with defined key word combinations
-Research gate
-Google Scholar
Hand Searching of reference lists of relevant articles
Keywords: Orthodontic Chin cup, chin cap, chin-cup, chin-cap, Class 3 malocclusion, Mandibular prognathism
Data Collection
1) Google scholar: Has high level of artificial intelligence and rich with articles. Saving search results are possible but selecting each article at a time. Boolean search is possible and words like ‘chin cup’ and ‘chin-cup’ are recognized as the same word. Moreover, ‘chin cap’ and chin cup’ are auto-linked i.e., both have the same search results even though the other could be mentioned in the article.
Final search keywords: chin cup and class III malocclusion and mandibular prognathism.
Results: 409 articles
keywords: chin cup, chin cup and class III malocclusion, chin cup and mandibular prognathism
2) Medline via Pubmed: Level of artificial intelligence of the search engine is very high. Boolean operator is possible, therefore keywords combinations were also used to filter results further.
Search keywords: ((chin-cup) AND (class iii malocclusion)) NOT (maxillary protraction) not (facemask) Filters: Clinical Trial, Meta-Analysis, Randomized Controlled Trial – 4 articles
Search: (mandibular prognathism treatment) NOT (surgery)- 100 articles
Search: (((orthodontic) AND (extra oral appliances)) and (chin cup) or chin cap or chin-cap or chin-cup - 200 articles
Search: (((((chin cap) OR (chin cup)) OR (chin-cap)) OR (chin-cup)) AND (orthodontic)) AND (class 3 malocclusion) - 39 articles
Search: (chin cap) OR (chin cup) OR (chin-cup) OR (chin-cap) OR (contemporary chin cup) - 200 articles
Search: (orthodontics) AND (chin cup) - 10 articles
Total result: 553 articles
3) Science direct: Logged in through personal Warwick account and that allowed access to more full text articles. However, it has limited flexibility in the use of combined keywords (Boolean search is not possible).
Search keywords: were limited to ‘chincup’ (a one word) as the term ‘chin cup’ had many irrelevant articles results and filtration is very limited.
Results: 37 articles
4)Research gate: Linked it to personal Warwick email account to increase articles accessibility. It has several new articles but no filtration options. Moreover, many of the articles do not have available full text. Several full text articles were requested but only one author responded.
Results: 35+
5) Cochrane Library: it has good advanced search options but few relevant articles available.
Results: 5 articles
6) ISI web of knowledge: search engine does not recognize Boolean commands, therefore allowed only defined keywords combination. Search filtration is also very limited and not user-friendly.
Results: 11 articles
7) Hand search: References list of relevant articles were hand search for other relevant papers.
Results: 35 articles
The results from these different search engines were combined and managed as per PRISMA flow chart considering the below inclusion/exclusion criteria:
Inclusion criteria
- Papers originally written in English
- Studies published between years 2010- November 2020
- Peer-reviewed papers as high as possible in the hierarchy of evidence such as randomized control trial, controlled clinical trials, and Cohort studies
- Studies involving only healthy and symmetric facial growth pattern.
- Clinical studies
- Researches about the treatment of growing skeletal CLIII individuals with normal maxilla and prognathic mandible, and that used the chin cup therapy.
Exclusion Criteria
- Papers published before year 2010 and after November 2020
- Original Papers not published in English language.
- Peer-reviewed papers low in the hierarchy of evidence such as case reports and case series studies
- Animal studies
- Non-clinical studies
- Medically compromised individuals
- Studies including candidates with diseases, disabilities, asymmetric facial growth pattern or Tempro-mandibular joint dysfunction
- Papers on the treatment of CLIII malocclusion that do not include chin cup therapy
- Papers about CLIII malocclusion, with deficient maxilla and normal mandible.
The purpose of the above exclusion criteria was to aid in filtering and limiting the vast database about the topic, based on the decided PICO and also due to time restraints of this review Figure 1.
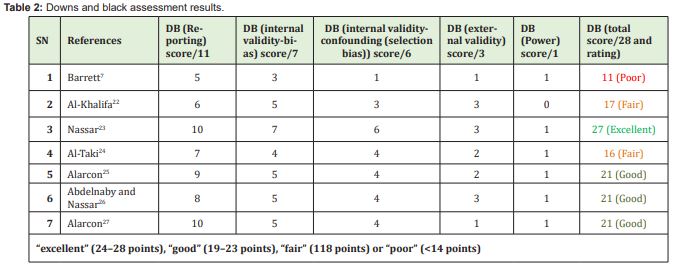
The risk of bias assessment tool used was the modified Downs and Black checklist and scale to assess the methodological quality of both randomized and non-randomized studies.10 The scale provides numeric score out of a maximum of 28 points and it categorizes scores into Excellent, Good, Fair, and Poor. This option makes it easier for researchers to select the most appropriate articles for further analysis using Critical Appraisal Skills Programme (CASP 2018). Only highly evidenced based articles were identified and reviewed against the aim of the study.
Data Storage
During the research process data was saved on personal laptop hard drive and backed up to personal email archive. Both these were security protected. On completion of the study, data and the final work was converted to a Adope Acrobat Format (PDF) format and saved on the personal laptop hard drive, email archive and a Compact Disc (CD-ROM) for long term storage.
Dissemination
Angle Orthodontist Journal has an open access and has one of the highest impact factor results on www.journalguide.com website, hence it is chosen to be approached in the event of publication. Therefore, based on the approval of the MD955 course directors at Warwick University, this study can be published if it met the journal’s criteria. There is also a high possibility that the present review be presented to staff or other dental professionals in peer review, staff meetings, or clinical network meetings or lectures.
Ethical approvals
This study is a review of existing data that was readily available, hence did not require approvals from Biomedical & Scientific Research Ethics Committee (BSREC) and NHS or National Research Ethics Service (NRES).11
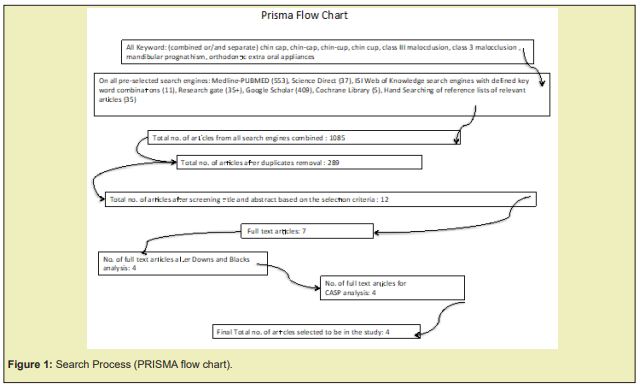
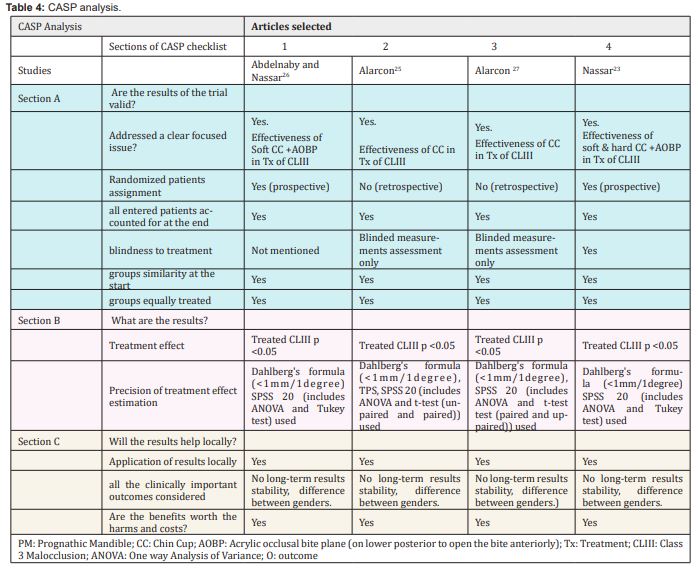
Risk of bias assessment: Downs and black analysis
Out of the 1085 articles shown in table 1, only 7 were found relevant to be assessed for the risk of bias by Downs and Black scale (D&B results displayed in Table 2). From the 7 articles, 1 achieved an ‘excellent’ score, 3 ‘good’, 2 ‘fair’, and 1 ‘poor’. It was decided to exclude the studies with the ‘fair’ and ‘poor’ scores, to critically appraise only the studies with the least risk of bias. Consequently, only four papers (Table 3) were retrieved and critically appraised by CASP (Table 4).
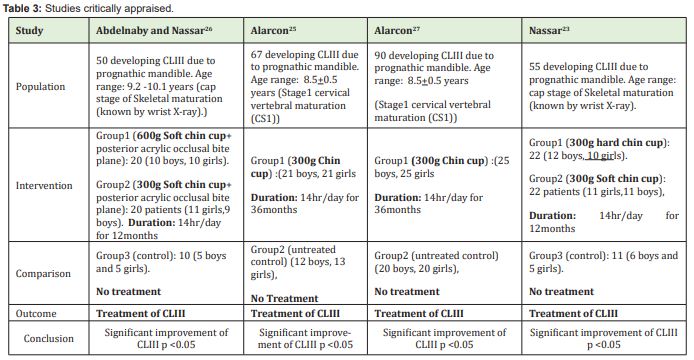
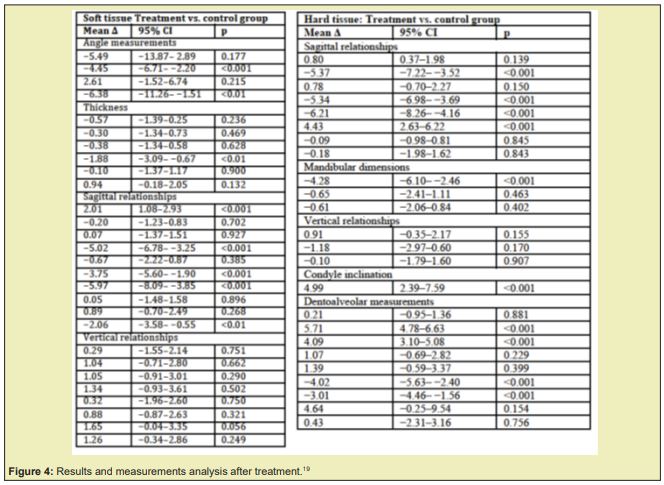
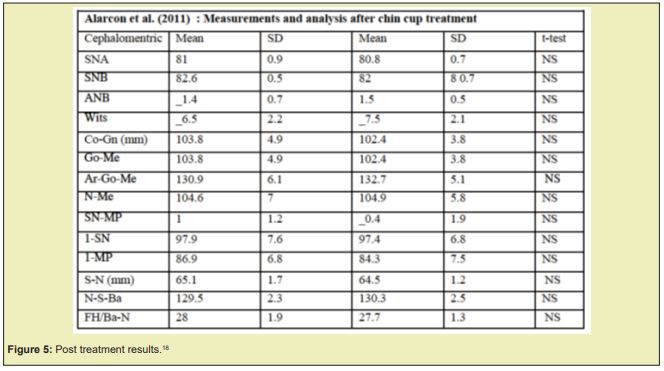
As per the results of the four studies reviewed (tables of studies’ results shown on Figures 2-5, chin cup is proved to have significantly modified shape of the mandible, and was effective in the treatment of Class 3 malocclusion with mandibular prognatism.

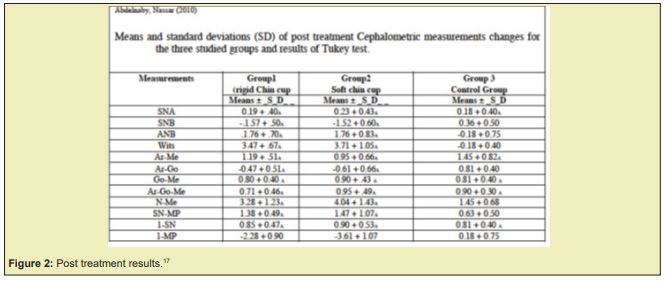
Nasser revealed that chin cup resulted to clockwise rotation of the mandible, and that significantly increased anterior facial height (N-Me) and mandibular plane angle (SN-MP). These findings were supported by previous studies.12-17
The same study also showed that hard and soft chin cup have almost the same dental and skeletal effects, though the soft chin cup produces significantly (p< 0.05) more retroinclination of the lower incisors.
In addition, Abdel Naby17found that the reduction in ramus height was significantly more (P <0.05) when a force of 600g per side of a chin cup was used, rather than 300g of force.
The purpose of the present literature review was to assess the effectiveness of chin cup therapy in the treatment of CLIII malocclusion with prognathic mandible. The study material final selection relied on D&B and CASP analyses, which filtered the collected database and resulted in the retrieval of only four RCTs’ and non-RCTs’ articles to be the core of this investigation. Alarcon,18,19 Abdelnaby17 and Nassar12 had generally low risk of biased conclusions and their precision in the data and statistical analyses was remarkable. Efforts were made to address confounders, method errors and statistical errors. I am not aware of better errors management systems, other than those they adopted. However, some weaknesses were identified and that shall be discussed while interpreting the CASP analysis results.
CASP analysis interpretation
Interestingly, the articles had similar CASP analysis results mainly because of having coincidently common authors. For instance, José Antonio Alarcón (Department of Stomatology, School of Dentistry, University of Granada, Granada), was one of the authors in two of the studies, and Essam Abdelalim Nassar (Associate Professor, Department of Orthodontics, Faculty of Dentistry, Mansoura University, Mansoura, Egypt) was an author in the other two papers.
Differences between the papers appeared in the 3 sections of analysis (Section A, B, and C), but mainly related to: assessment of skeletal maturation, type of chin cup, co-intervention, randomized patients’ assignment, precision of treatment effect estimation, and results.
Skeletal maturation assessment and mean age of the studies’ population
An effective orthopedic treatment of skeletal Class 3 malocclusion is likely expected if the therapy is administered before the pubertal growth peak (Campbell 1983). Furthermore, individuals of the same age can exhibit different stages of skeletal development. Maturation also varies between genders (San Roman, 2002). Consequently, it is preferable to confirm the patients’ skeletal maturation stage before the commencing of treatment, rather than deciding a mean age range. Abdelnaby, Nassar12,17 used the wrist X-ray assessment method to confirm patients’ skeletal developmental stage. While Alarcon18,19 adopted the cervical vertebral maturation staging system, which can estimate the maturation level in both males and females. It relies on the concavity of the lower border of the cervical vertebrae body, which is the best vertebral parameter to assess maturity (San Roman, 2002). This technique can replace the wrist X-ray, and reduces unnecessary radiation exposure to the child (San Roman, 2002). Authors of the appraised papers did not justify their choice of the skeletal maturation identification system they used. In spite of that, the cervical vertebral maturation staging systems seems more convenient as it depends on cephalometric x-rays, which are mandatory at the commencing and cessation of any orthodontic treatment to asses effects of the interventions. Therefore it minimizes the X-ray radiation the child is exposed to, unlike the wrist X-ray method.
Chin cup type
Alarcon18,19 mentioned the brand of the occipital chin cup but not its firmness (hard or soft). Abdel Naby17 specified the use of soft chin cup type, while Nassar12 compared the effects of the two chin cup types (soft and hard) on the patients. Anyhow, hard and soft chin cups are reported to have similar dental and skeletal effects, but the soft type produced significantly (p< 0.05) more retroinclination of the lower incisors. Giancotti,20 and Mitani21 also observed the retro inclination in their studies. Practically, the hard chin cup is readily available in the market and its effects on the skin of the chin, and the dento-alveolar structures are more predictable than that of the soft chin cup. Applying allergen-free moisturizer or a very thin layer of sponge on the tissue bearing area of the cup may reduce the skin discomfort and laceration at the pressure spot.
Randomization
Abdelnaby & Nassar (2010) and Nassar12 were prospective studies therefore randomising treatment assignment was possible.17 This was not applicable for Alarcon18,19 for being retrospective, but blinding during the measuring stage and, data analysis was performed likewise. Randomization and blinding of treatment assignment during the selection process and measurements analysis, reduce the risk of bias in a research, hence raises the studies’ level of significance, and the quality of evidence.
Co-intervention
Abdelnaby & Nassar (2010) and Nassar12 used posterior acrylic bite plates to disengage the bite anteriorly, which is in crossbite. This disocclusion allows a normal unrestricted growth of the maxilla and also allows the mandible to a retrude more easily during chin cup treatment. Sargod,22 Ngan23 and Watnick24 supported the same. In contrast, Alarcon (2011) and Alarcon (2015) did not consider it. Based on my personal clinical experience disocclusion tends to speed alignments of the dental arches during orthodontic treatment.
Precision of treatment effect estimation
All the papers followed the same analytical process (shown in box below) but with some differences in the details:
Cephalometric X-rays tracing à randomized and blinded Retracing à Dahlberg’s formula used to assess method error à Statistical analysis of variables using software package SPSS (One way Analysis of Variance (ANOVA) and Tukey test/ t-test were utilized to detect significance between-group differences for all variables. Tukey test also identifies statistical errors).25
Alarcon (2011) and Alarcon (2015) retraced (operator blinded) randomly selected 25 cephalometric x-rays and re-digitalized them after interval of 10 days, then assessed method errors by using Dahlberg’s formula. Nassar (2018) applied the same but for 30 x-rays and 20 days interval. Abdelnaby & Nassar (2010) just mentioned retracing cephalometric X-rays, without specifying their number, randomisation, or the gap interval.
Moreover, Alarcon (2011) transferred the digitized Cephalometric tracing to tpsDIG software (TPS)26,27 to analyse and compare cephalometric landmark’s superimpositions. Alarcon (2015), Abdelnaby & Nassar (2010) and Nassar12did not mention any digital system for the same purpose. Involving the TPS might not affect the significance of measurements, but should probably provide a more illustrative image of the changes that occurred in the measured object’s shape.28
The force magnitude applied on the mandible through the chin cup was 300g per side in all the trials, except for Abdelnaby & Nassar (2010). The latter used 600g force also in one of its groups to compare its effect to that of 300g, and as a result, the 600g force was found to produce significantly more ramus height reduction than the 300g. Deguchi29 compared short-term chin-cup therapy (500g force for 31 months), to long term therapy (250g to 300g force for 86 months) and concluded that long-term treatment resulted in a significant improvement in class III malocclusion. Katashiba30 conducted a similar comparison as Deguchi,30-32 but a group wore the chin cup (250 g to 300g force) 14 hours per day for 2 years and the other group (500g force) wore it over night time only. Katashiba30 observed that aggressive protocol of chin cup therapy was the recommended solution for developing class III malocclusions. Furthermore, the concept of applying light continuous force in orthodontics is usually applied in my practice as it is more controllable and minimizes the risk of harmful excessive forces, especially when patients continue wearing the orthodontic appliance but irregular with the follow-up visits.
In regards to the wearing time of the device, the four trials instructed their patients to wear it fourteen hours per day. In literature, wearing a chin cup for 10-14 hours daily, could affect the direction of chin growth, as the direction alteration is linked to the period of force exerted on the mandible.33,34
On the other hand, ethnicity of the patients was not considered. It is worthy to know the ethnicity of a study’s population as the normal skeletal and soft tissues manifestations, and development may vary. For example, individuals with Asian ancestry may present with baseline characteristics that are different from others.9 Despite that, this did not seem to have a significant impact the studies as the populations were selected from the registry of public universities, which usually treat the locals of that place. In that case, I can assume the patients were of the same race in each of the investigations.
Other controversies that were known by the researchers of the four trials, but were not assessed or evaluated were the duration of treatment and the long-term stability of the treatment results. Alarcon (2011) and Alarcon (2015) reported satisfactory results after treatment duration of 36 months, while Nassar (2018), and Abdelnaby & Nassar (2010) observed similar effects after only 12 months of chin cup therapy. The description of the post treatment clinical presentation is not illustrated clearly, and does not confirm the achievement of CLI jaws relationship. Choices of their treatment period were not justified, hence length of the therapy remains questionable. In a systematic review, Nowrin (2017) stated that long-term (more than 5yrs or until the end of juvenile growth) use of chin cup significantly retards mandibular growth and is effective in patients with severe Class III malocclusion.35
In regards to long-term mandibular modification stability, Sugawara,36 noted that chin cup effects on the mandible were not stable on the long term, as the patient’s normal growth pattern of the mandible continues, thus causing a relapse if chin cup therapy was ceased before skeletal maturation. In addition, when recommending a long duration treatment phase, patient’s compliance should be considered, as it is likely to have a significant impact on the success of the intervention. A definitive conclusion about this controversy may not be possible due to the limited research on the topic.
In general, the four investigations concluded that chin cup significantly improved the clinical manifestation of Class 3 malocclusion due to skeletal and dentoalveolar modifications. Alacron (2015) and Nassar (2018) also found that the soft tissues followed the skeletal changes during chin cup therapy. Furthermore, Alacron (2015) mentioned that the soft tissue measurements might be less reliable than those of hard tissues, due to variation in its thickness and tension, thus potentially concealing significant changes.37 This fact about soft tissues measurements demands a vivid comparison of the preclinicsl clinical and radiographic (soft and hard tissues) manifestations.38-56
Finally, this review did answer the controversy about the effectiveness of chin cup in the management of Class 3 malocclusion. It also proved that chin cup therapy has favorable impacts on facial soft tissues. Nevertheless, it made me interested in conducting future research about the long-term stability of treatment results post chin cup therapy.
Basal Cell Carcinoma is relatively common in daily clinical practice, which is why offering a definitive and practical treatment for the patient with low costs for the healthcare system is essential. This increasingly common pathology in our environment can be treated in different ways, but undoubtedly, surgical treatment has the lowest long-term recurrence rates. For this reason, a flap that is easy to perform and requires local tissues from the patients is ideal in our environment. The bilobed transposition flap in most cases meets the needs of the disease and the skills of the surgeon.
None.
None.
The author confirms that this article content has no conflict of interest.
- 1. Peter W Ngan, Jae Hyun Sung. Esthetics and Biomechanics in Orthodontics. Chapter 14 - Treatment Strategies for Developing and Nondeveloping Class III Malocclusions. 2015;p.246–293.
- 2. Moher D Liberati A, Tetzlaff J. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009;6(7):e1000097.
- 3. Burleson: How does an orthodontic chin cup work?
- 4. Weinberger BW. Orthodontics; an historical review of its origin and evolution, including an extensive bibliography of orthodontic literature up to the time of specialization. St. Louis, The C.V. Mosby Company. 1926.
- 5. Graber LW. Chin cup therapy for mandibular prognathism. Am J Orthod. 1997;72:23–41.
- 6. Zurfluh MA, Kloukos D, Patcas R, et al. Effect of chin-cup treatment on the temporomandibular joint: a systematic review. Eur J Orthod. 2015;37(3):314–324.
- 7. Watkinson S, Harrison JE, Furness S, et al. Orthodontic treatment for prominent lower front teeth (Class III malocclusion) in children. Cochrane Database Syst Rev. 2013;(9):CD003451.
- 8. Flavio Andres Uribe, Ravindra Nanda (2015): Management of Open-Bite Malocclusion, in Esthetics and Biomechanics in Orthodontics (Second Edition).
- 9. Mousoulea S, Tsolakis I, Ferdianakis E, et al. The Effect of Chin-cup Therapy in Class III Malocclusion: A Systematic Review. Open Dent J. 2016;10:664–679.
- 10. Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health. 1998;52(6):377–384.
- 11. National Research Ethics Service: Research & Impact Services.
- 12. Nassar EA, Hafez AM, Abdelnaby YL. Soft vs hard chin cup effects in management of Class III malocclusiona. A randomized control clinical trial. Egyptian Dental Journal. 2018;64(83):90.
- 13. Lee W. Graber. Chin cup therapy for mandibular prognatism. From the Center for Human Growth and Development and Department of Anatomy, University of Michigan Ann Arbor, Mich., USA. American journal of orthodontics. 1977;72(1):23–41.
- 14. Deguchi T, Kuroda T, Minoshima Y, et al. Craniofacial features of patients with Class III abnormalities: growth-related changes and effects of short-term and long-term chincup therapy. Am J Orthod Dentofacial Orthop. 2002;121(1):84–92.
- 15. Sugawara J, Mitani H. Facial growth of skeletal Class III malocclusion and the effects, limitations, and long-term Dentofacial adaptations to chincap therapy. Semn Orthod. 1997;3(4):244–254.
- 16. Proffit WR, Fields HW Jr, Sarver DM. Contemporary Orthodontics. 4th edn. St Louis, MO: Mosby. 2007.
- 17. Abdelnaby YL, Nassar EA. Chin cup effects using two different force magnitudes in the management of Class III malocclusions. Angle Orthod. 2010;80(5):957–962.
- 18. Alarcón JA, Bastir M, Rosas A, et al. Chincup treatment modifies the mandibular shape in children with prognathism. Am J Orthod Dentofacial Orthop. 2011;140(1):38–43.
- 19. Alarcón JA, Requena MA, Delgado AC, et al. Association between changes in soft and hard tissue after early chin cup treatment. J Orofac Orthop. 2015;76(3):225–239.
- 20. Giancotti A, Maselli A, Mampieri G, et al. Pseudo-Class III malocclusion treatment with Balters' Bionator. J Orthod. 2003;30(3):203–215.
- 21. Mitani H, Fukazawa H. Effects of chincap force on the timing and amount of mandibular growth associated with anterior reversed occlusion (Class III malocclusion) during puberty. Am J Orthod Dentofacial Orthop. 1986;90(6):454–463.
- 22. Sargod SS, Shetty N1, Shabbir. Early class III management in deciduous dentition using reverse twin block. Journal of indian society of pedodontics and preventive dentistry. 2013;31(1):56–60.
- 23. Ngan P, Hu AM, Fields HW. Treatment of Class III problems begins with differential diagnosis of anterior crossbites. Pediatr Dent. 1997;9(6):386–395.
- 24. Watnick SS. Inheritance of craniofacial morphology. Angle Orthod. 1972;42(4):339–351.
- 25. Felipe de Mendiburu. agricolae: Statistical Procedures for Agricultural Research. R package version.2019;3–1:2019.
- 26. TpsDIG software (tpsSeries, J. F. Rohlf, Department of Ecology and Evolution, State University of New York at Stony Brook. 2004.
- 27. Rohlf FJ, Slice D. Extensions of the Procrustes method for the optimal superimposition of landmarks. Syst Biol. 1990;39:40–59.
- 28. Riolo ML, Moyers RE, McNamara JA, et al. An atlas of craniofacial growth. Craniofacial Growth Series. Monograph 2. Ann Arbor: Center for Human Growth and Development; University of Michigan. 1974.
- 29. Deguchi T, McNamara JA. Craniofacial adaptations induced by chincup therapy in Class III patients. Am J Orthod Dentofacial Orthop. 1999;115(2):175–182.
- 30. Katashiba S, Deguchi T, Kageyama T, et al. The aggressive chin cup protocol (14 h/day for 2 years with excellent compliance) depends on commitment to overcorrection of the skeletal class III malocclusion. Orthodontic Wave. 2006;65(1):57–63
- 31. Deguchi T, Kuroda T, Hunt NP, et al. Long-term application of chincup force alters the morphology of the dolichofacial Class III mandible. Am J Orthod Dentofacial Orthop. 1999;116(6):610–615.
- 32. Deguchi T, Kitsugi A. Stability of changes associated with chin cup treatment. Angle Orthod. 1996;66(2):139–145.
- 33. Wendell PD, Nanda R, Sakamoto T, et al. The effects of chin cup therapy on the mandible: a longitudinal study. Am J Orthod. 1985;87(4):265–274.
- 34. Gökalp H, Kurt G. Magnetic resonance imaging of the condylar growth pattern and disk position after chin cup therapy: a preliminary study. Angle Orthod. 2005;75(4):568–575.
- 35. Ritucci R, Nanda R. The effect of chin cup therapy on the growth and development of the cranial base and midface. Am J Orthod Dentofacial Orthop. 1986;90(6):475–483.
- 36. Sugawara J, Asano T, Endo N, et al. Long-term effects of chincap therapy on skeletal profile in mandibular prognathism. Am J Orthod Dentofacial Orthop. 1990;98(2):127–133.
- 37. Arman A, Toygar TU, Abuhijleh E. Profile changes associated with different orthopedic treatment approaches in Class III malocclusions. Angle Orthod. 2004;74(6):733–740.
- 38. Abu Alhaija ES, Richardson A. Long-term effect of the chincap on hard and soft tissues. Eur J Orthod. 1999;21(3):291–298.
- 39. Chong YH, Ive JC, Artun J. Changes following the use of protraction headgear for early correction of Class III malocclusion. Angle Orthod. 1996;66(5):351–362.
- 40. Irie M, Nakamura S. Orthopedic approach to severe skeletal Class III malocclusion. Am J Orthod. 1975;67(4):377–392.
- 41. Ishikawa H, Nakamura S, Kim C, et al. Individual growth in Class III malocclusions and its relationship to the chin cap effects. Am J Orthod Dentofacial Orthop. 1998;114(3):337–346.
- 42. Lin HC, Chang HP, Chang HF. Treatment effects of occipitomental anchorage appliance of maxillary protraction combined with chincup traction in children with Class III malocclusion. J Formos Med Assoc. 2007;106(5):380–391.
- 43. Maher Fouda. Chin cup for treatment of growing class III patient. From Faculty of Dentistry, Mansoura university. 2016.
- 44. Chatzoudi MI, Ioannidou Marathiotou I, Papadopoulos MA. Clinical effectiveness of chin cup treatment for the management of Class III malocclusion in pre-pubertal patients: a systematic review and meta-analysis. Prog Orthod. 2014;15(1):62.
- 45. McNamara JA Jr. An orthopedic approach to the treatment of Class III malocclusion in young patients. J Clin Orthod. 1987;21(9):598–608.
- 46. Mitani H, Sakamoto T. Chin cap force to a growing mandible. Long-term clinical reports. Angle Orthod. 1984;54(2):93–122.
- 47. Mitani H, Sato K, Sugawara J. Growth of mandibular prognathism after pubertal growth peak. Am J Orthod Dentofacial Orthop. 1993;104(4):330–336.
- 48. Mitani H. Early application of chincap therapy to skeletal Class III malocclusion. Am J Orthod Dentofacial Orthop. 2002;121(6):584–585.
- 49. M Al Muzian. Msc ortho, Extraoral Orthodontic Appliances. 2017.
- 50. Auconi P, Scazzocchio M, Caldarelli G, et al. Understanding interactions among cephalometrics variables during growth in untreated Class III subjects Author Notes. European Journal of Orthodontics. 2017;39(4):395–401.
- 51. Sakamoto T, Iwase I, Uka A, Nakamura S. A roentgenocephalometric study of skeletal changes during and after chin cup treatment. Am J Orthod. 1984;85(4):341–350.
- 52. Sandra Durcevic in Data Analysis Your Modern Business Guide To Data Analysis Methods And Techniques.
- 53. Tahmina K, Tanaka E, Tanne K. Craniofacial morphology in orthodontically treated patients of class III malocclusion with stable and unstable treatment outcomes. Am J Orthod Dentofacial Orthop. 2000;117(6):681–690.
- 54. Uner O, Yüksel S, Uçüncü N. Long-term evaluation after chincap treatment. Eur J Orthod. 1995;17(2):135–141.
- 55. Uçüncü N, Uçem TT, Yüksel S. A comparison of chincap and maxillary protraction appliances in the treatment of skeletal Class III malocclusions. Eur J Orthod. 2000;22(1):43–51.
- 56. Liu ZP, Li CJ, Hu HK, et al. Efficacy of short-term chincup therapy for mandibular growth retardation in Class III malocclusion. Angle Orthod. 2011;81(1):162–168.

