Background: Studies have shown sufficient evidence to associate a subtype of Human papillomavirus (HPV) 16 with oro- pharyngeal cancers and these organisms are typically transmitted through sexual contact making HPV the world’s most common sexually transmitted infection. Fortunately, quadrivalent and bivalent vaccines for HPV infections have shown some evidence of effectiveness in reducing the incidence of oro-pharyngeal cancers (OPC). The knowledge level of people concerning HPV infection, related cancers and vaccines can influence the incidence and prevalence of the infection and its consequences.
Aim: The study aims to assess the knowledge level of university students concerning HPV infections, related cancers and vaccines.
Methods: A cross-sectional survey was conducted in April, 2017, in the University of Health and Allied Sciences (UHAS). A total of 399 respondents aged 16 to 30 years were interviewed using semi-structured questionnaire. SPSS Windows version 22.0 was used for data analysis.
Results: Of the 399 respondents, 278(69.7%) were females while 121(30.3%) were males. Most (93.2%) were aged 18- 24 years; 87.7% had heard of HPV mostly during a lecture at UHAS (80.7%). Findings showed that only 8% and none of the respondents correctly associated HPV with OPC and cancer of the head and neck region respectively. Additionally, 59.4% of the respondents were not aware of vaccination as a preventive tool; with yet 60.7% being unaware of its availability in Ghana. Also, none of the respondents were vaccinated against HPV; and the main reasons for non-vaccination included: unaware of vaccines availability in Ghana and lack of knowledge on males’ vaccination.
Conclusion: The majority of respondents were aware of HPV, but general knowledge about HPV infections and vaccinations were low. The study highlights the need for education on HPV infections; and the availability of vaccines for HPV prevention in Ghana for both males and females.
Keywords: Oro-pharyngeal cancer, Cervical cancer, Human papilloma virus, Vaccination
Human papillomavirus (HPV) are part of a diverse family of viruses capable of causing epithelial tumors in humans; including cervical cancers which is the second most frequent cancer in women worldwide and a variable proportion of certain non-cervical malignancies, including vulvar, vaginal, penile, anal, and oro-pharyngeal cancers (OPC).1,2 With over 150 different subtypes of HPV that have been identified worldwide, types 16 and 18 are associated with the onset of 70% of cervical cancers worldwide.3-5 In addition to HPV, smoking and alcohol are well known risk factors of OPC.6
The prevalence of HPV in women is most common before age 30, with a second incidence peak later on in life. In men, however, the prevalence is more stable across all ages. Most infections are asymptomatic with most women (75-80%) infected with HPV at some time during their life; but longitudinal studies have shown that 90% of infections are cleared within one to two years.
Human Papillomavirus transmission occurs primarily during sexual activity, oral HPV is mainly transmitted through oral sex or open-mouth kissing, whereas genital HPV is transmitted through skin-to-skin contact during sexual activity, and not the exchange of body fluids like in other (bacterial) STIs. This means that the use of condoms confers some extent of protection, but not completely. Other transmission routes known for HPV include vertical transmission from mother to infant, a risk which is greater after vaginal than caesarean birth.
Relationship to Oro-Pharyngeal Cancers
In 2012, the International Agency of Research of Cancer (IARC) declared that there was sufficient evidence to associate a subtype of HPV 16 with oral cancers.7 Additionally, these HPV-related oral cancers differ from HPV-negative tumors or cancers in their clinical response and overall survival rates.8,9
A total of 99% of HPV infections in oro-pharyngeal carcinoma (OPC) are related to highrisk types 16, 18, 31, or 3310, with HPV 16 as the most common subtype and HPV 33 accounting for up to 10% of cases.10,11
Current changes in sexual practices, including first sexual experience at an earlier age, high number of sexual partners, and high probability of oral sex, may be associated with the increasing prevalence of HPV infection12 and thus OPC.
Recent development has produced two prototypes of prophylactic vaccines against HPV infections namely: a quadrivalent vaccine (Gardasil) and a bivalent vaccine (Cervarix), that both protect against the two most common cancer-causing HPV types (HPV-16 and HPV-18). Gardasil additionally confers immunity to HPV-6 and HPV-11, the virus types most responsible for ano-genital warts (condyloma)
To date, there is little information in the scientific journal regarding Ghanaian men and women’s knowledge and attitudes about HPV infection, cervical cancer and the roles that they may play in the development of cervical cancer and other HPV associated cancers. Thus, this work aims to determine the knowledge of Human Papillomavirus infections, related cancers and vaccines in male and female tertiary university students.
To determine the knowledge level of human papillomavirus infections and vaccines in male and female undergraduate students of UHAS.
1. To assess the knowledge level of HPV infection, related cancers and mode of transmission.
2. To assess the knowledge level of HPV infection prevention, vaccines and HPV vaccine uptake.
A cross-sectional survey was carried out among students of the University of Health and Allied Sciences on the Trafalgar and Sokode campuses. The sampling frame for all levels 100 and 200 students were obtained from the school records for all the five schools represented at the Sokode and Trafalgar campuses; and using a simple random sampling method, random numbers were generated with the aid of a computer and selected students were given self-administered questionnaires to fill after consenting to participate in the study.
Well-structured questionnaire was used to collect demographic information and assess the knowledge level of the study population on HPV infections, related cancers and vaccines.
Data was analyzed with the Statistical Package for Social Sciences (SPSS) version 22.0 for windows software.
Socio-demographic Characteristics of Respondents
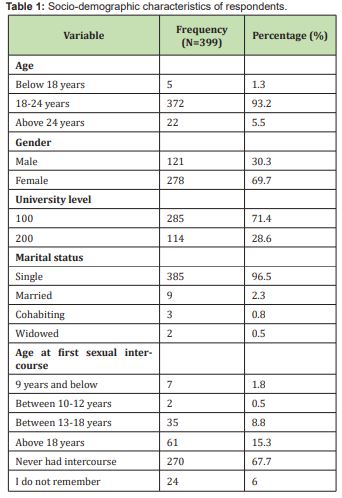
In all majority (93.2%) of the respondents were aged between 18-24 years; and 5.5% aged above 24 years while 1.3% were aged below 18 years. This pre-suggests that majority of the respondent are within their reproductive ages and therefore may be sexually active. With respect to sex, 69.7% of the respondents were females and 30.3% were males. Also 71.4% of the respondents were in level 100 and 28.6% in level 200.
With respect to religion, 93.7% were Christians, 5.3% Moslems, 0.5% traditionalists and 0.5% Buddhists.
Analysis of marital status showed that 96.5% of the respondents were single, 2.3% married, 0.8% cohabiting and 0.5% widowed.
With respect to age at first sexual intercourse, 67.7% had never had sex, 15.3% had sex at age above 18 years, 8.8% had sex between 13-18 years, 6.6% could not remember the time of sex, 1.8% had intercourse below 9 years and 0.5% had first intercourse between 10-12years Table 1.
Knowledge about HPV Infections
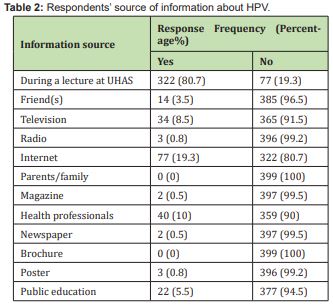
It is noteworthy that 87.7% of respondents have ever heard of human papilloma virus infections before, while 12.3% had not; information on HPV infections were mainly received: during a lecture at UHAS (80.7%), on television (8.5%), through the internet (19.3%) and from health professionals (10%) Table 2.
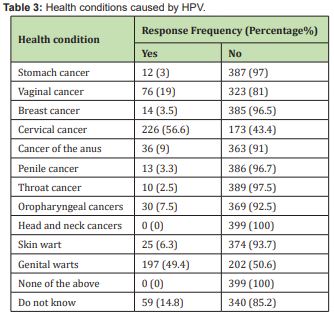
Enquiries on knowledge of health conditions that can be caused by or associated with HPV infections, showed that 56.6% of respondents correctly associated HPV with cervical cancer and 49.4 % with genital warts. But only 7.5% of respondents correctly associated HPV with OPC Table 3.
Knowledge about HPV Transmission Routes
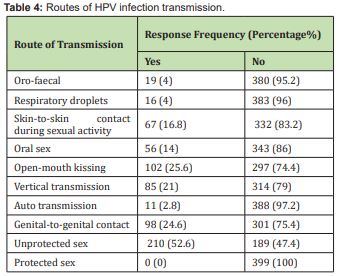
On enquiries on the mode of transmission of HPV: 52.6% said transmission occurs through unprotected sex, vertical transmission -21%, open-mouth kissing- 25.6%, genital -to-genital contact -24.6% and skin-to-skin contact during sexual activity-16.8%.
HPV Infection Prevention
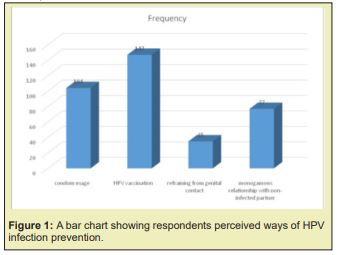
When asked if HPV infections can be prevented, majority (91.5%) of respondents said ‘yes’ while 8.5% said ‘no’. however, questioned on ways of HPV prevention, only 36.8% of respondents identified vaccination as a means; 26.1% said condom usage will prevent infection; 19.3% were for ‘monogamous relationship with non-infected partner’ while the remaining 8.8% were for ‘refraining from sexual contact’ Figure 1.
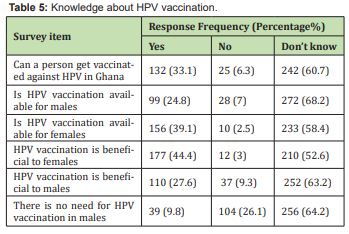
Knowledge of HPV Vaccination and Vaccination Status
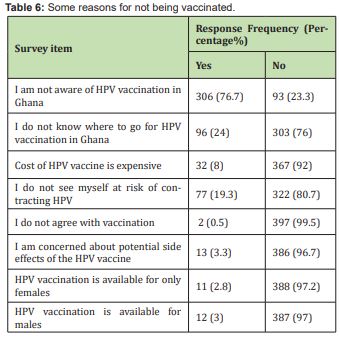
When subjects were asked if they had ever heard of HPV vaccination, 59.4% of respondents were not aware of vaccination, while 40.6% of respondents were aware. On vaccination status of respondents against HPV infections, all the respondents had not been vaccinated as at the time of the study. Some of reasons given for nonvaccination included not aware of availability of HPV vaccination in Ghana and lack of knowledge on where to access such service and others didn’t see themselves at risk of contracting HPV and some males didn’t know that men could also be vaccinated against HPV Tables 5,6.
Respondents’ Knowledge about HPV Infections and Transmission
Results from the study showed that more than three quarter of the subjects (87.7%) were aware of HPV infections and related cancers. This high value of awareness can be attributed to the fact that, these subjects are within the university environment and have access to first hand and reputable sources of information including lectures, mass media, print media and the internet. The finding is similar to the 65% that was reported in Benin among health workers;13 another study of undergraduate students in Ibadan had found that 71% of the students were aware of HPV infections and cervical cancer.14 However very high levels of awareness have been reported in Accra, Ghana15 (90%) among female university staff.
The study’s findings also showed that only 8% and none of the respondents correctly associated HPV with OPC and cancer of the head and neck region respectively; however, no studies have been carried out in Ghana yet to compare with.
In our study we found that 68.7% of the respondents were aware that HPV infections is transmissible; this is similar to reports by Agyakwa, (2015) in the University of Cape Coast where 74.2% of the respondents were aware that HPV infection is transmissible. However, there is a low level of knowledge about the routes of transmission of HPV, in this regard, only about half of the students (52.6%) were able to correctly associate HPV transmission with unprotected sex while 16.8%, 21% and 24.6% were able to associate transmission with skin-to-skin contact, vertical transmission and genital-genital contact respectively.
Respondents’ Knowledge about HPV Infection Prevention and Vaccine Uptake
Solid evidence from randomized trials demonstrated that the two available HPV vaccines prevent cervical cancers 16,17 and other non-cervical lesions and cancers including oro-pharyngeal cancers.18-20 This study shows that majority (91.5%) of the students were aware that HPV infections can be prevented. However only 36.8% knew that HPV infections can be prevented by vaccination; others ascribed mode of prevention to condom usage (26.1%), monogamous relationship with non-infected partner (19.3%) and refraining from sexual contact with an infected person (8.8%).
With respect to knowledge of vaccine and uptake of vaccination we found that only 33.1% of the respondents knew that they could be vaccinated against HPV infections and that it is available in Ghana. The low knowledge of HPV vaccination could be due to the fact that knowledge about HPV does not necessarily correspond to a correct understanding of the disease and its prevention methods.
The value and importance of education and information are essential for prevention efforts to be effective and equally important for personal decision-making. Currently, there is a deficit in literacy as it pertains to health. Several studies have linked literacy as an important predictor of health behaviour.
Vaccination status further showed that none of the respondents were vaccinated against HPV infections. This is consistent with findings in Cape Coast where none of the respondents were vaccinated against HPV infection.21 Nonetheless, our study showed that respondents were not vaccinated because they were unaware (76.7%) of availability of such vaccination in Ghana. However, the two main HPV vaccines (Gardasil & Cervarix) are very much available; and children particularly girls, should be given the vaccine between the ages of 10 and 12 before they become sexually active; and young adolescent boys are not exempted from this exercise; as earlier studies (Kaba et al., in 2014), have found that males had a high index of HPV in a subset of head and neck cancer cases. Thus, men are equally at risk of developing malignant tumours by the high-risk HPV variants.
The findings of this research showed a high level of awareness of HPV infections but low knowledge level of HPV infections, related cancers and HPV transmission modes. Additional findings showed low knowledge levels of HPV infection prevention, vaccination and vaccine uptake among the study population.
The university should endeavour to concentrate on informing students more about HPV infections, its link to cervical cancer and other cancers; transmission modes and strategies to prevent transmission, coupled with making vaccination available to them. Education on HPV vaccine should also include information about its safety and its benefit to prevent cervical and oro-pharyngeal cancers.
None.
None.
Authors declare that there is no conflict of interest.
- 1. Walboomers JM, Jacobs MV, Manos MM, et al. Human papillomavirus is a necessary cause of invasive cervical cancer worldwide. J Pathol. 1999;189:12–19.
- 2. van der Marel J, Berkhof J, Ordi J, et al. Attributing oncogenic human papillomavirus genotypes to high-grade cervical neoplasia: which type causes the lesion?. Am J Surg Pathol. 2015;39(4):496–504.
- 3. Bosch FX, Lorincz A, Muñoz N, et al. The causal relation between uman papillomavirus and cervical cancer. J Clin Pathol. 2002;55(4):244–265.
- 4. Muñoz N, Bosch FX, de Sanjosé S, et al. Epidemiologic classification of human papillomavirus types associated with cervical cancer. N Engl J Med. 2003;348:518–527.
- 5. de Villiers EM, Fauquet C, Broker TR, et al. Classification of papillomaviruses. Virology. 2004; 324(1):17–27.
- 6. Sun JR, Kim SM, Seo MH, et al. Oral cancer incidence based on annual cancer statistics in Korea. J Korean Assoc Oral Maxillofac Surg. 2012;38:20–28.
- 7. IARC Working Group on the Evaluation of Carcinogenic Risks to Humans. IARC monographs on the evaluation of carcinogenic risks to humans: IARC monographs. A review of human carcinogens. B. Biological agents. Lyon. International Agency for Research on Cancer. 2012;100B:278–280.
- 8. Fakhry C, Westra WH, Li S, et al. Improved survival of patients with human papillomavirus-positive head and neck squamous cell carcinoma in a prospective clinical trial. J Natl Cancer Inst. 2008;100(4):261–269.
- 9. Dayyani F, Etzel CJ, Liu M, et al. Meta-analysis of the impact of human papillomavirus (HPV) on cancer risk and overall survival in head and neck squamous cell carcinomas (HNSCC). Head Neck Oncol. 2010;2:15.
- 10. Kim KS, Park SA, Ko KN, et al. Current status of human papillomavirus vaccines. Clin Exp Vaccine Res. 2014;3:168–175.
- 11. Snow AN, Laudadio J. Human papillomavirus detection in head and neck squamous cell carcinomas. Adv Anat Pathol. 2010;17(6):394–403.
- 12. Heck JE, Berthiller J, Vaccarella S, et al. Sexual behaviours and the risk of head and neck cancers: a pooled analysis in the International Head and Neck Cancer Epidemiology (INHANCE) consortium. Int J Epidemiol. 2010;39(1):166–181.
- 13. Ghararo EP, Ikeanyi E N. An appraisal of the level of awareness and utilization of the pap smear as a cervical cancer screening test among female health workers in a tertiary health institution. Int J Gynaecol cancer. 2006;16(3):1063–1068.
- 14. Ayinde OA, Omigbodun AO, Ilesanmi AO. Awareness of cervical cancer, Papanicolaou's smear and it's utilisation among female undergraduates in Ibadan. Afr J Repro Health. 2004;8(3):68–80.
- 15. Adanu R. Cervical cancer knowledge and screening in Accra, Ghana. J Women’s Health Gend Based Med. 2002;11(6):487–488.
- 16. Lehtinen M, Paavonen J, Wheeler CM, et al. Overall efficacy of HPV-16/18 AS04- adjuvanted vaccine against grade 3 or greater cervical intraepithelial neoplasia: 4-year endof- study analysis of the randomised, double-blind PATRICIA trial. Lancet Oncol. 2012;13(1):1989–1999.
- 17. Munoz N, Kjaer SK, Sigurdsson K, et al. Impact of human papillomavirus (HPV)- 6/11/16/18 vaccines on all HPV-associated genital diseases in young women. J Natl Cancer Inst. 2010;102(5):325–339.
- 18. Giuliano AR, Palefsky JM, Goldstone S, et al. Efficacy of quadrivalent HPV vaccine against HPV Infection and disease in males. N Engl J Med. 2011;364(5):401–411.
- 19. Palefsky JM, Giuliano AR, Goldstone S, et al. HPV vaccine against anal HPV infection and anal intraepithelial neoplasia. N Engl J Med. 2011;365(17):1576–1585.
- 20. Crosignani P, Stefani A, Fara GM, et al. Towards the eradication of HPV infection through universal specific vaccination. BMC public health. 2013;13:642.
- 21. Ofori GP, Ebu NI, John M, et al. Knowledge, Attitude and Practices of Cervical Cancer Screening Among Female Nursing Students of University of Cape Coast, Ghana. Poster 130, 2014.

