Because of change, the pressure in a cabin in an airplane and the potential eye problem can be caused. The ophthalmologist determined that patients who had undergone cataract surgery or vitreoretinal surgery on long-haul flights should be informed for clarification. Neuro-ocular vestibular dysfunction (NOVD), ischemic optic neuropathy, exacerbating diabetic macular edema have also been reported in association with the disorder eye occurred while on a plane. The International Headache Society (IHS) has classified eye pain that occurs while traveling by plane as a headache type since 2013. In this paper, we reported a patient who received cataract surgery (lens extraction / intraocular lens IOL) without any complications having a postoperative vision of 6/6, 6 months prior, when performing a flight for more than 20 hours his eye was diagnosed a retinal detachment with blind vision and restored vision after one month of treatment.
Keywords: Airplane, Eye problem, NOVD, HIS
Because of the pressure change in the cabin in an airplane and the potential eye problem can be caused. The eye doctors who identify the patient undergone cataracts or vitreoretinal surgery traveling on long flights should be advised for clarification.1 Neuro-ocular vestibular dysfunction (NOVD), ischemic optic neuropathy, aggravation of diabetic cystoid macular edema have been also reported regarding the ocular disorders to occur during air travel. International Headache Society (IHS) has classified ocular pain which occurred in the air traveling as a type of headache since 2013.2 Diagnostic criteria of “airplane headache” (AHA) include fulfilling criteria at least 2 attacks, including ‘’1. severe pain during airplane travel lasting less than 30 min, with at least 2 of these ‘’unilateral pain, fronto-orbital location (frontoparietal pain may occur), the pain of jabbing or stabbing quality (pulsating may occur)’’; ‘’2. no accompanying symptoms’’; ‘’3. not attributed to other disorders’’
Vasodilation in brain vessels developed in an attacking company of AHA can be generated. by prostaglandin E2.3 Although there is no special methodological or prophylactic treatment for AHA, it has been shown that certain medications including pain relievers, nonsteroidal anti-inflammatory drugs, or triptans can have beneficial effects as prophylactic therapy Passive eye problems due to changing air pressure in aircraft takeoffs and landings and were divided into 2 parts: an anterior segment of the eye and posterior segment of the eye. The most common eye problem among airplanes traveling in the anterior segment of the eye such as the dry surface (20%) due to dehydration of the air in the air-conditioner, and dry skin and eyes often appear. In addition, there may be eye with contact lenses, cramping or head pain, watery eyes, and lens intolerance applying the primary source of oxygen under the focal lens.4,5 The rapid drop in atmospheric pressure during flight can increase the compatible pressure. However, this change usually does not cause problems in patients with glaucoma during aircraft transfers because the aircraft cabin has artificial atmospheric pressure being checked and this often compensates for the malfunction pressure develops at high altitudes.6 The posterior segment of the eye on patients undergoing surgery from glaucoma, lens extraction with IOL implant, retinal detachment, and vitrectomy are likely to be affected by the changing air pressure. Optic neuropathy is caused by ischemia, which can be aggravated. Diabetic macular edema has also been reported with eye disorders that occur during long plane travel. Furthermore, it has been speculated that central retinal artery occlusion or events ischemia of the other eye may occur due to reactive vasoconstriction or ischemic changes during elevation movement are a worrying symptom
In this paper, a patient who received cataract surgery (lens extraction/intraocular lens IOL) without any complications having a postoperative vision of 6/6, 6 months prior was reported. When performing a flight for more than 20 hours the eye was diagnosed with a retinal detachment with blind vision and restored vision after one month of treatment.
A 57 years old male patient. Visual acuity = Left eye normal 6/6. Right eye = Cataract surgery with IOL implant. History of right eye: Visual acuity after surgery: 1 week was 6/60 and 3 weeks was 6/6. Six months after cataract surgery, he took a flight longer than 20 hours. A few days later when came back home, his vision was counting fingers 1 foot. General examination, pulse 75/min, blood pressure 130/70mmHg, blood sugar 100mg%. No history of cardiovascular disease, diabetes. Check the retina, the position of the tear near the macula, the detached retina. B Ultrasound images of the retina in both eyes are showed in Figure 1.
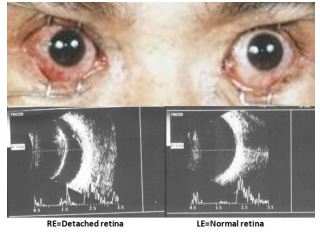
Diagnosis: RE=Retinal detachment.
Treatment: Retinal surgery, Retinopexy pneumatics: Inject a bubble of air into the central part of the vitreous cavity. The bubble pushes the retinal area into the eyeball wall, blocking the flow of fluid into the space behind the retina. Keep the head in a certain position for up to a few days to a few weeks to keep the bubbles in the proper position. The bubble finally reabsorbed by itself by the end of the third week. Three months later, the vision regained 6/9.
This is a male case, 57 years old, with no accompanying systemic disease. Lens extraction with IOL implant without complication and visual acuity is 6/6 for 3 weeks after surgery. Six months later he took a long airplane traveling for 20 hours. When he came back his home he became blind by retinal detachment. Risk factors for retinal detachment include severe nearsightedness, retinal tear, trauma, family history, as well as complications from cataract surgery, and low eye pressure. In this case, it might be combined cataract surgery involving low intraocular pressure during a long flight.6
Retinal detachment occurs when fluid under tissue accumulates between the retina nerve and retinal pigment epithelium. This process can happen in three ways. A mechanism involved in the appearance of a rupture in the retina allows the lens to enter the sub-retinal cavity directly.
The second mechanism involves proliferating membranes on the surface of the retina or vitreous bodies. Directed retinal detachment can also be caused by post-traumatic or surgical retinal proliferation.7
Other disorders: The air turbulence can cause an open wound in the corneal incision area due to swallowing saliva and vomiting, or a severe increase in eye pressure due to dilated gas in the eye and consequently obstruction of the central retinal artery. Therefore, these passengers should not travel immediately after cataract surgery and must be seated by a seat belt. Trip delay for about two to six weeks after ocular injection of sulfur hexafluoride (SF6) and perfluoropropane (C3F8), has been recommended, respectively.8,9
Prevention: Patients with known risk factors for retinal detachment should receive a dilatation exam followed by scleroderma, usually annually. Protective glasses are recommended for people with high myopia when participating in contact sports. Patients undergoing cataract surgery should be advised of the importance of reporting symptoms of retinal tear and detachment.
Medication is also essential in aortic disorders and ocular immobilization when needed. Or artificial tears, wearing sunglasses instead of contact lenses, drinking more water, turning the air conditioner blowing direction to the side instead of turning your face, and resting while reading in-flight can reduce or prevent discomfort. Exercises that include compression on the pain site, Valsalva maneuver, enlarging the earlobes, chewing or yawning can reduce pain intensity by 25%.2
Refer to the American Academy of Ophthalmology:10 Whether restoring vision after eye surgery or having a specific condition affects the patient's vision means that the patient should fly. If you have questions about your eye health, you should talk with your own ophthalmologist. But it's important to know that sometimes flying in a plane can actually endanger your eyes. If you have undergone any type of surgery, talk to your doctor about your travel plans. Find out what to expect after surgery, so you know if you are having a serious symptom. Consider staying close to home for a few days - or recommended by your doctor - in case of problems arise. And always keep a follow-up visit so your doctor can make sure you are healing as expected. If you have been diagnosed with an eye condition, ask your ophthalmologist if there are activities you should limit or avoid. Make sure you understand your doctor's recommendations and ask questions about specific activities if you are unsure. Consider how long it takes to take a few days, weeks, or months to avoid possible complications especially during a long flight doctor's encouragement and your understanding of these matters.
The case mentioned above, a blind retinal detachment after a long airplane traveling on the patient with six months prior cataract surgery /IOL implant having very good vision, with no abnormalities in heath had been detected before. More research is needed on these issues. Because of change, the pressure in a cabin in an airplane and the potential eye problem can be caused. Especially cases of retinal and optic nerve disease as severe myopia, retinal detachment, or intraocular surgery with complications have been warning. The identification of ophthalmologists on these patients should be further investigated to recommend a safe time for traveling on a long-distance flight.
None.
No funding or grant support was received for this work.
No financial disclosures.
- 1. Turgut B. Ocular problems associated air traveling. Adv Ophthalmol Vis Syst. 2018;8(2):80-83.
- 2. Kaiserman I, Frucht Pery J. Anterior ischemic optic neuropathy after a trans-Atlantic airplane journey. Am J Ophthalmol. 2002;133(4):581-583.
- 3. Headache Classification Committee of the International Headache Society (IHS). The International Classification of Headache Disorders, 3rd edition (beta version). Cephalalgia. 2013;33(9):629-808.
- 4. Bui SBD, Gazerani P. Headache attributed to airplane travel: diagnosis, pathophysiology, and treatment–a systematic review. J Headache Pain. 2017;18(1):84.
- 5. Norbäck D, Lindgren T, Wieslander G. Changes in ocular and nasal signs and symptoms among air crew in relation to air humidification on intercontinental flights. Scand J Work Environ Health. 2006;32(2):138-144.
- 6. Bagshaw M, DeVoll JR, Jennings RT, et al. Medical guidelines for airline passengers.
- 7. Retinal detachment
- 8. Retinal Detachment. EyeWiki.
- 9. Houston S, Graf J, Sharkey J. Commercial air travel after intraocular gas injection. Aviat Space Environ Med. 2012;83(8):809-810.
- 10. Dan Gudgel. Learn what eye conditions should keep you on the ground and which won’t interfere with air travel. Can I Fly With This Eye? American Academy of Ophthalmology.

