Purpose: In this study, we aimed to retrospectively evaluate the demographic data, clinical features, laboratory data, precipitating causes of diabetic emergencies, complications in the follow-up of adult patients who applied to our hospital due to diabetic emergencies.
Methods: The study included patients aged 18 years and older referred to a tertiary endocrine center with diabetic ketoacidosis (DKA), hyperosmolar hyperglycemic state (HHS) hypoglycemia between January 2010 and May 2018.
Results: The study was carried out with 165patients, 69(41.8%) males, and 96(58.2%) females. The mean age of the patients was 43.8±20.4(18- 88). Of these patients, 77% (n=127) had DKA, 17% (n=28) had HHS and 6% (n=10) had hypoglycemia. Of the patients 55.2% (n=91) were type 1 DM, 44.8% (n=74) were type 2DM. When the precipitating causes of diabetic emergencies were examined, 32.7%(n=54) poor adherence to treatment and 32.1%(n=53) infection of the patients were involved. The new diagnosis was DM in 10.9% of the patients (n=18). The most common complication after treatment was hypopotassemia with 38.7% (n=60), but no complication was observed in the majority of patients (54.8%). In our study, total mortality was 1.8% and 11.1% in HHS patients. No mortality was found in DKA and hypoglycemia patients.
Conclusion: Diabetic ketoacidosis is more common in DM patients than in other diabetic emergencies. Approximately 11% of patients do not have a known diagnosis of diabetes. Poor adherence to treatment and infection are the most important precipitating causes of the diabetic emergency. The mortality rate is very low with early diagnosis and correct treatment.
Keywords: Diabetic emergencies, Diabetic ketoacidosis, Hyperosmolar hyperglycemic state, Hypoglycemia
Diabetic emergencies include Diabetic ketoacidosis(DKA), Hyperosmolar Hyperglycemic State(HHS), and hypoglycemia. The common features of these diseases are their high mortality rates and being the most common reason for diabetic patients to apply to the emergency department.1 In addition to mortality risks, diabetic emergencies are also important with their high cost.2 DKA, HHS and hypoglycemia are serious complications of DM that require rapid diagnosis and treatment. DKA, and HHS are characterized by hyperglycemia and insulinopenia.3 Clinically, these two conditions differ only with the degree of dehydration and the severity of metabolic acidosis. The total mortality of DKA in society is below 1%. The mortality rate in patients with HHS is approximately 10 times higher than that associated with DKA. The prognosis in these patients is proportional to the severity of dehydration, the presence of co-morbid diseases, and age.4,5
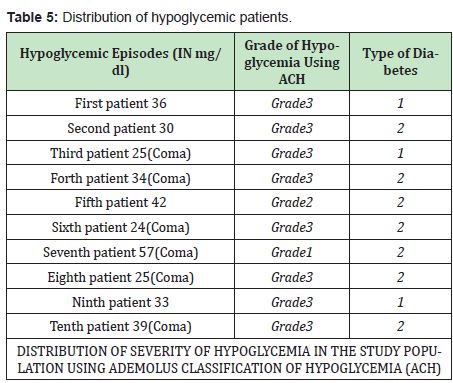
Hypoglycemia was defined as a blood glucose level of 70mg/dl and below. Hypoglycemia classification was made according to the Ademolus Hypoglycemia Classification (ACH). (Grade 1-Mild hypoglycemia glucose 55-70mg/dl, grade 2-moderate hypoglycemia glucose 40-54mg/dl, grade-3 severe hypoglycemia glucose 10-39 mg/dl, grade-4 very severe hypoglycemia glucose<10mg/dl).6 The aim of this study was to retrospectively evaluate the demographic data, clinical characteristics, laboratory data, precipitating factors causing diabetic emergencies, complications during follow-up, and recovery times of patients followed up in a tertiary endocrine center for diabetic emergencies.
Patient selection: In this study, patients over 18 years of age who presented to tertiary endocrine center between January 2010 and May 2018 and were diagnosed with DKA, HHS, or hypoglycemia were included.
Study design: Patients with Type 1 Diabetes and Type 2 Diabetes were included in the study. Patients with positive anti-GAD antibodies and patients with low c-peptide levels (<0.5ng/ml) were included in the study as type 1 DM.The demographic characteristics, physical examination findings, laboratory data, duration of diabetes, precipitating factors leading to a diabetic emergency, home treatment regimens, recovery times, and post-treatment complications of patients diagnosed with diabetic emergencies were retrospectively analyzed from the hospital registry system. Diagnostic criteria for DKA were accepted as admission glucose level>250mg/ dl, blood gas pH<7.30 and HCO3<18mmol/L, and at least 2+ ketones in urinalysis. For HHS, the admission glucose level was>600mg/dl, osmolarity>320mosm/kg, and the absence or low rate of ketone in urinalysis. Hypoglycemia was defined as a blood glucose level of 70mg/dl and below. Hypoglycemia classification was made according to the AdemolusHypoglycemia Classification (ACH).6
Laboratory tests: The glucose, pH, HCO3 (bicarbonate), K (potassium), Na (sodium), Cl (chlorine), urea, creatinine, WBC, HbA1c, and c-peptide levels of the patients were recorded from the hospital registry system. In addition, serum osmolarity and anion gap were calculated in line with these data.
Ethics committee form: This study was approved by Dicle University Faculty of Medicine Non-Invasive Clinical Research Ethics Committee (Decision number:37Date: 06.06.2018). Statistical analysis: Statistical analysis of the results obtained in the study was performed using the Statistical Package for Social Sciences (SPSS) 22.0 statistical software package. Descriptive statistics for continuous variables, which were emphasized, were expressed as mean±standard deviation, minimum and maximum values, while categorical variables were expressed as numbers and percentages. Pearson correlation test was used to determine whether there was a relationship between two numerical measurements, and One-Way ANOVA test was used in the comparative analysis of any numerical variable in more than two groups. In addition, Chi-square test was used in the analysis of categorical variables. Continuous variables were compared with Student t-test, and discontinuous variables were compared with Mann-Whitney U test. A p<0.05 in these tests was considered statistically significant.
Of the 165patients who were admitted to our hospital due to diabetic emergencies and included in the study, 76.9%(n=127) were diagnosed with DKA, 16.9%(n=28) HHS and 6%(n=10) were diagnosed with hypoglycemia. In our study, 58.2% of the patients were female (F), 41.8% were male (M), and the F/E ratio was found to be approximately 1.4. Female patients were 57.5%(n=73) of DKA patients, 63%(n=17) of HHS patients, and 50%(n=5) of hypoglycemia patients.
The mean age of all patients was 43.8±20.4 (18-88), and the mean age in patients diagnosed with DKA was 37.2±17.1(18-84), and 69.4±11.5(49-88) in HHS patients. In patients diagnosed with hypoglycemia, it was 57.9±18.7(23-82).(Table 1)

55.2% (n=91) of the patients were type 1 DM, and 44.6% (n=74) were type 2 DM. While the rate of type 1 DM was 70% (n=89) and type 2 DM rate was 30% (n=38) in DKA patients, all HHS patients were patients with a diagnosis of type 2 DM. 20% (n=2) of hypoglycemia patients were type 1 DM, and 80% (n=8) were type 2 DM.
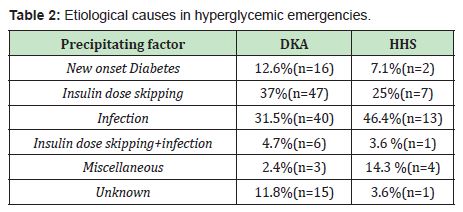
When the precipitating factors causing diabetic emergency are examined; In the first two places were skipping insulin doses with 32.7% (n=54) ,and infection with 32.1% (n=53). No underlying factor was found in 15.8% (n=26) of the patients, and 10.9% (n=18) were patients who had not been diagnosed before and were hospitalized as newly diagnosed diabetes. In 7 patients, there was a combination of infection and skipping insulin doses. In 7 patients, other causes such as cerebrovascular accident, acute coronary syndrome or heart failure were detected. In DKA patients with 37% (n=47), skipping insulin doses is the most common cause, while infection is the second most common cause with 31.5% (n=40), in patients with HHS, infection is the first with 46.4% (n=13), 25% (n=7) followed by skipping insulin doses.(Table 2)
When the patient’s unconscious condition was evaluated at the time of admission to the hospital, the consciousness was normal in 85 patients, and consciousness changes were observed in 80 patients, changing from consciousness blur to coma. Consciousness changes were found in 38,6% of DKA patients (n=49), 88,9% of HHS patients (n=24), and 60% of patients diagnosed with hypoglycemia (n=6).
In HHS patients, the level of urea and creatinine was significantly higher than DKA patients (p<0.001 and p<0.001). There was no significant difference between the potassium levels between the groups (p=0.563), but the sodium level was significantly higher in HHS patients (p<0.001). (Table 3)

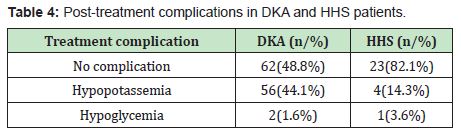
When patients were evaluated for post-treatment complications, no complications were developed in 54.8% (n=85) of the total 155 patients. It was determined that 48.8% of DKA patients (n=62) and 82.1% of HHS patients (n=23) did not develop any complications after treatment. In 44.1% of DKA patients (n=56), hypopotassemia was developed, while HHS patients were found to have developed hypopotassemia in 14.3% (n=4). (Table 4)
Blood glucose levels, state of consciousness and ACH classification of hypoglycemic patients are shown in Table 5.
In this study, the most common cause of patients who have applied to the hospital due to a diabetic emergency was identified as diabetic ketoacidosis. In addition, about one-third of patients with diabetic ketoacidosis were patients with type 2 DM. When diabetic ketoacidosis is not properly treated or there is a delay in diagnosis/ treatment, morbidity and mortality are high. Although diabetic ketoacidosis type 1 DM is more frequently seen, it is also encountered in type 2 DM, up to one-third.7,8 In our study, the accelerating factors that lead to diabetic emergencies can be listed as follows: skipping insulin doses, non-compliance with dietary treatment, and non-compliance with drug therapy are the main reasons for the majority of the patients. This suggests that awareness of diabetes treatment and diabetic emergency among patients should be increased and that the healthcare team should make an effort on the treatment of diabetes of the patient.
When the accelerating factors causing the diabetic emergency are examined; Infection, skipping insulin dose, and newly diagnosed DM are the most common causes in most clinical trials.9 Similar results were obtained in our study, and the rates of infection and insulin dose skipping were very close to each other. However, when only DKA patients were considered, insulin dose skipping was greater than for other factors. DKA is mostly observed in young patients and HHS is more common in the elderly. Mortality is higher in HHS.10,11 In our study, the mean age of DKA was found to be in the 30s and the average age in HHS was 60 years. Although diabetic hypoglycemia is mostly seen in patients using insulin, it can also be seen in patients using oral anti-diabetic drugs. It is known that sulfonylurea (SU) group drugs are risky in terms of hypoglycemia. As a matter of fact, in our study, all patients who were diagnosed with hypoglycemia and used OAD had an SU group drug.
In hyperglycemic emergencies, plasma creatinine levels may be high at admission. Among the reasons for this, dehydration due to osmotic diuresis of glucose is prominent, as well as the presence of diabetic nephropathy and ketoacidosis.11 In our study, the mean creatinine level at presentation was calculated as 1.5±0.7mg/dl in DKA patients and 2.3±1.0mg/dl in HHS patients. We think that this is due to the presence of comorbid diseases in type 2 diabetic patients and the more frequent development of nephropathy. In hyperglycemic emergencies, hypopotassemia is frequently observed at the time of diagnosis and as a treatment complication.12,13 In our study, the most common treatment complication was found to be hypopotassemia. To avoid this complication, patients should be given potassium replacement as appropriate. In our study, no treatment complication developed in more than half of the patients.
The limitations of the study can be listed as follows. Retrospective design, lack of control group, and lack of data arising from the retrospective study. In conclusion, DKA, which is one of the diabetic emergencies, is frequently seen in patients with type 1 diabetes. Skipping insulin doses, infection, and newly diagnosed DM are the most common precipitating factors leading to a diabetic emergency. For this reason, we believe that patient education and awareness- raising on blood glucose monitoring and infection prevention strategies should be an important focus in the prevention of hyperglycemic emergencies. The mortality rate is very low with early diagnosis, correct treatment, and close follow-up of patients.
None.
None.
Authors declare that there is no conflict of interest.
- 1. Kitabchi AE, Umpierrez GE, Miles JM, et al. Hyperglycemic crises in adult patients with diabetes. Diabetes Care. 2009;32(7):1335–1343.
- 2. Umpierrez G, Korytkowski M. Diabetic emergencies-ketoacidosis, hyperglycaemic hyperosmolar state and hypoglycaemia. Nat Rev Endokrinol. 2016;12(4):222–232.
- 3. Fayfman M, Pasquel FJ, Umpierrez GE. Management of Hyperglycemic Crises: Diabetic Ketoacidosis and Hyperglycemic Hyperosmolar State. Med Clin North Am. 2017;101(3):587–606.
- 4. Pasquel FJ, Umpierrez GE. Hyperosmolar hyperglycemic state: a historic review of the clinical presentation, diagnosis, and treatment. Diabetes Care. 2014;37(11):3124–3131.
- 5. Muneer M, Akbar I. Acute Metabolic Emergencies in Diabetes: DKA, HHS and EDKA. Adv Exp Med Biol. 2021;1307:85–114.
- 6. Adegbenga B Ademolu. Analysis of Hypoglycemic Episodes in Diabetics in Africans Using Ademolus Classification of Hypoglycemia (ACH). Acta Scientific Medical Sciences. 2019;3(3):138–145.
- 7. Eledrisi MS, Elzouki AN. Management of Diabetic Ketoacidosis in Adults: A Narrative Review. Saudi J Med Med Sci. 2020;8(3):165–173.
- 8. Newton CA, Raskin P. Diabetic ketoacidosis in type 1 and type 2 diabetes mellitus: clinical and biochemical differences. Arch Intern Med. 2004;164(17):1925–1931.
- 9. Umpierrez GE, Kitabchi AE. Diabetic ketoacidosis: risk factors and management strategies. Treat Endocrinol. 2003;2(2):95–108.
- 10. Gouni-Berthold I, Krone W. Diabetic ketoacidosis and hyperosmolar hyperglycemic state. Med Klin (Munich). 2006;101 Suppl 1:100–105.
- 11. MacIsaac RJ, Lee LY, Mc Neil KJ, et al. Influence of age on the presentation and outcome of acidotic and hyperosmolar diabetic emergencies. Intern Med J. 2002;32(8):379–385.
- 12. Rewers A. Acute Metabolic Complications in Diabetes. In: Cowie CC, Casagrande SS, Menke A, Cissell MA, Eberhardt MS, Meigs JB, Gregg EW, Knowler WC, Barrett-Connor E, Becker DJ, Brancati FL, Boyko EJ, Herman WH, Howard BV, Narayan KMV, Rewers M, Fradkin JE, editors. Diabetes in America. 3rd ed. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases (US); 2018 Aug. CHAPTER 17.
- 13. Dhatariya KK, Glaser NS, Codner E, et al. Diabetic ketoacidosis. Nat Rev Dis Primers. 2020;6(1):40.

