The clinical symptoms of endometriosis, an illness characterized by ectopic endometrium (glands and stroma) outside the uterus, are mainly dysmenorrhea, dyspareunia, cyclic urinary symptoms and infertility. Although imaging modalities such as pelvic ultrasound can identify and localize endometriotic deposits in the ovary (endometrioma) and in bladder wall, diagnosis of the disease is impossible where such imaging modalities are unavailable or where clinicians are not trained to clinically diagnose endometriosis during consultation. Especially in sub-Saharan Africa, clinicians should be familiar with certain predisposing risk factors for endometriosis such as early age at menarche, shorter menstrual length and low body mass index. Delay in the diagnosis of endometriosis not only prolongs the duration of suffering, pain and discomfort but also lowers quality of life and increases cost of treatment. This article focuses on how gynecologists and clinicians in sub-Saharan Africa can easily identify the symptomatology of endometriosis. Clinical presentations of endometriosis in Black African women may not be different from presentations among Caucasian women. Though a confusing illness for the patient and for the clinician, at least, African gynecologists, clinicians and general practitioners can have a suspicion of endometriosis when a Black African woman presents with a combination of infertility, pelvic pain, dysmenorrhea and dyspareunia. This article discusses various conditions associated with endometriosis in adolescent women and in women in child-bearing age group.
Keywords:Black african women, Cyclic urinary symptoms, Diagnosis, Dysmenorrhea, Dyspareunia, Endometriosis, Endometrioma, Infertility, Menarche, Symptomatology
Abbreviations: BMI: Body Mass Index; CAS: Current Awareness Service; MeSH: Medical Subject Headings; PubMed: Public/Publisher MEDLINE; Medline: Medical Literature Analysis and Retrieval System online; IVF: In-Vitro Fertilization; UNDP: United Nations Development Program; WHO: World Health Organization
Endometriosis is the presence of tissues from the inner lining of the uterus (glands and stroma) outside the uterus that generate prolonged and degenerative inflammatory reactions, scar tissue and adhesive pathology which usually deform female patient’s pelvic morphology.1 Endometriosis impacts one in every ten women of reproductive age, affecting about 200 million women globally.2 Between 40% and 50% of women with endometriosis will have infertility and approximately 30%-40% of women with infertility have endometriosis.3 The non-malignant lesions of endometriosis are usually located internally and in most cases confirmed by observational laparoscopy as cysts, nodules, or implants at various parts of internal tissues or organs in either the pelvic or abdominal peritoneum, especially the uterosacral ligament, recto-vaginal septum, sigmoid colon, ureter and urinary bladder and even the vermiform appendix.4-8 Depending on the site of endometriosis, symtomatology of endometriosis may vary widely considerably, impinging on the overall corporal, psychological and social well-being of the patient.9 From this perspective, it is of primary importance for clinician, the first point of contact for the woman, to patiently listen to and carefully take the history of the woman’s complaints, probing her obstetric and gynecologic history, sexual history, family history as well as anxieties and possible stigmatization in the context of African background of infertility. It is possible that the patient consults at Primary Health Care level in the town or village and clinicians in this setting should also consider endometriosis from the history given by the patient. It should be borne in however, that some women may present with no symptoms, thought there are tell-tail signs that can point to possible endometriosis in the patient.
In Tertiary Health Care facilities, the dominant approach to the diagnosis of endometriosis in Africa had been through surgical intervention and laparoscopic observation, and even then this illness is mostly missed by clinicians during consultation and by gynecologists and surgeons in the theater. The initial diagnosis of endometriosis requires a high index of suspicion. Although Galle10 observed that the clinic presentation of endometriosis is consequent upon
- 1. Location
- 2. Extent of disease
- 3. Severity of endometriosis
Which has poor correlation with the extent of the disease and although Galle10 further categorized symptoms of endometriosis into genital, ovulatory and reproductive dysfunctions, still certain salient points are missed in the clinic which lead to misdiagnosis of endometriosis even after evident menstrual dysfunction such as cyclic pelvic pain, dysmenorrhea and dyspareunia. Spaczinski and Duleba11 reported that endometriosis is a frequent maladie among women in child-bearing age, though its diagnosis is often baffling and problematic to clinicians. Delay in diagnosis has been a known characteristic of endometriosis, leading to worsening disease, pathology and complications, one of which is infertility. Laparoscopy, the often recommended gold standard for the diagnosis of endometriosis is not easily available or accessible in most part of sub-Saharan Africa and where it is accessible; the services may be quite expensive for easy affordability. Therefore, less invasive means of diagnosis are faster, cheaper and affordable with less complications. Clinical diagnosis and imaging can currently diagnose endometriosis in up to 80% of cased.12 In the end, especially in sub-Saharan Africa, a high index of suspicion of endometriosis is consequent upon detailed and painstaking clinical assessment,13 before any other vital steps such as laboratory investigations, histological assessment and surgical staging of the disease. Data on clinicians’ knowledge and accurate diagnosis of endometriosis is scarce in Africa. The notion that endometriosis is rare in the continent may be due to the fact that most clinicians are unaware of the salient points to look for and cogent questions to ask a patient with endometriosis. Perhaps, the true prevalence of endometriosis among infertile Black African women may be higher than reported. The under-reporting of endometriosis in Africa may be due to
- 1. Inadequate and under-manned facilities
- 2. Lack of specialized skills for complete pelvic assessment
- 3. Incognizance of varying types and appearance of endometriosis.
However, even though there are adequate facilities and staff with specialized skills, misdiagnosis of endometriosis will continue and those with the disease will continue to suffer unnecessarily if clinicians in Africa are not conversant with not only the clinical presentation of the disease but how to extract salient information on antecedent events, current evidence and probably quality of life of the affected patient.
This study aimed at increasing the index of suspicion of Care Providers in Africa by paying attention to relevant history taking with the aim of reducing the interval between onset of symptoms, diagnosis and possible management of endometriosis. The main objective of the study was to determine the characteristics that may be suggestive of endometriosis among Black African women presenting with infertility.
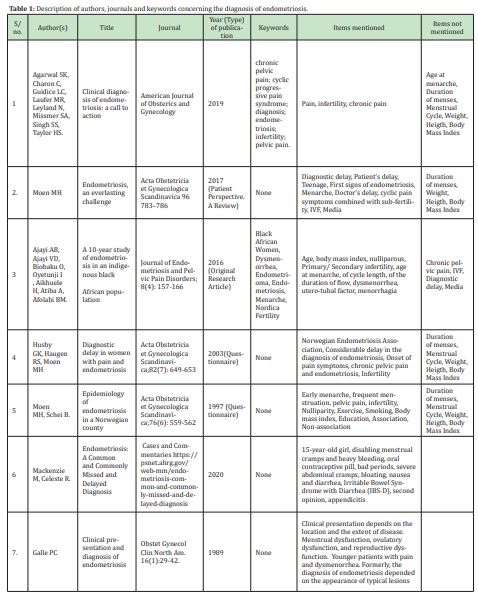
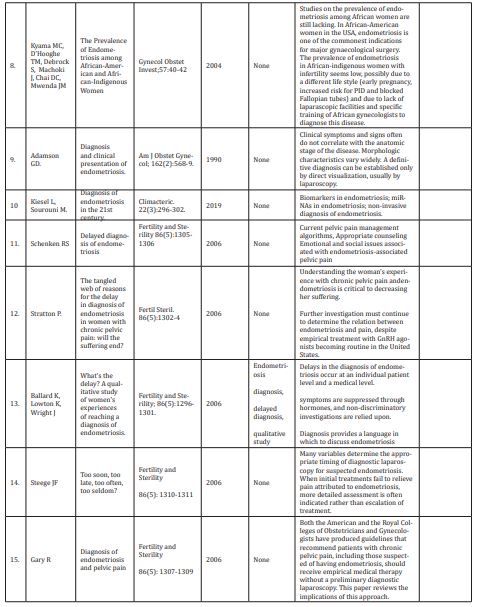
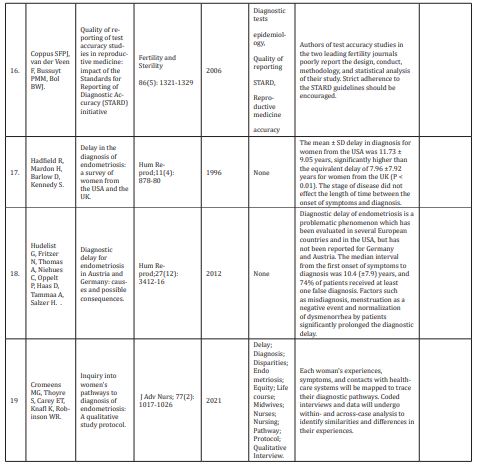
This study used bibliography to find out authors, journals and year of publication that mention specific items and symptoms that clinicians in African setting should probe for to ascertain a high index of suspicion of endometriosis in female clients. The bibliography covered also the region of the globe, individual papers, commissioned papers and other sources such as the internet, thesis and any government pronouncement on endometriosis. MeSH terms were used to look for specific words that clinicians should use to arrive at provisional diagnosis before surgical confirmation of endometriosis. Wiley Online Library, CAS, PubMed, Web of Science, ®Google Scholar and Cochrane Review were also accessed. These electronic databases were searched using the following key word strategy: clinical diagnosis of endometriosis, accurate diagnosis of endometrioma, diagnosis of pelvic pain, cyclic progressive pain, menarche and endometriosis, endometriosis and body mass index, delay in diagnosis, signs of endometriosis. Four MeSH (Medical Subject Headings) terms were also used where appropriate (i.e., endometriosis and infertility, Endometriosis and IVF (In-vitro fertilization), Endometriosis and Dysmenorrhea, Endometriosis and Menorrhagia) in combination with the key words – chronic pelvic pain, progressive pelvic pain, Endometriosis symptoms. Databases that were used were MEDLINE (1995-2021), PubMed (1995-2021) and Excerpta Medica (1995-2021). The purpose was to identify the progress of endometriosis management from the first contact with a clinician to the time of her discharge and to assess probing questions into definitive diagnosis of endometriosis. This method will be used in future medical training of clinicians in Africa for early diagnosis and management of the disease.
The following inclusion criteria were used:
- 1. The patients studied were selected for endometriosis and related topics such as endometrioma, ovarian cysts, adenomyosis, dysmenorrhea, menorrhagia, dyspareunia and other signs and symptoms of the disease
- 2. The paper should contain one form of clinical diagnosis or another
- 3. The paper must have been written within the past 30 years
- 4. All papers with sufficient information on endometriosis in sub-Saharan Africa reported in the published study to determine the prevalence of endometriosis in the region.
Exclusion criteria were
- 1. Pelvic pains not due to endometriosis
- 2. Dysmenorrhea, menorrhagia and dyspareunia of other origins
- 3. Papers older that 30 years.
The literature was searched for the period 1995 to 2021 for all related publications, reports or monograms in English language. Electronic searches of data bases such as Cochrane Library (www.cochranelibrary.com), Pub Med (https://pubmed.ncbi.nlm.nih.gov/12789123), MeSH (https://www.ncbi.nlm.nih.gov/mesh), and Medline were conducted using key words in various combinations to narrow or expand the search. The reference lists of original relevant research articles were also reviewed.
“Diagnosis of endometriosis” OR “Diagnosis of endometrioma” OR “Clinical diagnosis of endometriosis” OR “Clinical diagnosis of endometrioma” OR “Clinical presentation of endometrioma”OR “Delayed diagnosis of endometriosis” OR “Delayed diagnosis of endometrioma” OR “Differential diagnosis of endometriosis” OR “Differential diagnosis of endometrioma” OR “Clinical diagnosis of chronic pelvic pain” OR “Non-invasive diagnosis of endometriosis” OR “Diagnosis of endometriosis in Africa” OR “Endometriosis and Infertility, relevance of diagnosis” OR “Age at menarche and endometriosis” OR “Age at menarche and diagnosis of endometriosis” OR “Cycle length and diagnosis of endometriosis” OR “Body Mass Index and Endometriosis” OR “Body Mass Index and the Diagnosis of endometriosis” OR “Age and Endometriosis” OR “Age and the diagnosis of endometriosis” OR “Endometriosis” OR “Predictors of endometriosis” OR “Endometriosis and teenagers” OR “Teenage dysmenorrhea and endometriosis” OR “Diagnosis of endometriosis among teenagers” OR “Teenagers and Endometriosis”
Delayed diagnosis of any medical condition is one of the major causes of morbidity and mortality as well as a contributory factor to poor quality of life and high cost of hospitalization and medication. Always, there is usually a necessity for immediate and efficient recognition and treatment of a pathology to avoid serious adverse outcomes. When clinical diagnosis of endometriosis was searched for, 4,513 results were produced overall, between 2000 and 2021 with only 17 results in Africa within the same period, none of which described history taking for clinical diagnosis of endometriosis. In a systematic review, Maillard et al.,14 advised that diagnosis of vulvo-perineal endometriosis should be done with clinical exam, perineal ultrasound and pelvic MRI when available, though not much was said about the exact sequence of the clinical diagnosis. Byanyima15 reported the usefulness of imaging in a patient with thoracic endometriosis, but not much about the clinical diagnosis.
Clinical presentation of endometriosis in Black African women
Because most endometriotic implants are found on the uterus, ovaries, and posterior peritoneum, the patient usually presents with a history of progressively increasing pelvic pain and/or secondary dysmenorrhea. In a study of about 1,500 patients, Ajayi et al.,16 reported that the commonest presentation of endometriosis among Black African women are primary infertility, dysmenorrhea, menorrhagia and utero-tubal factors. Clinical presentation of endometriosis in Black African women may not be significantly different from that among their Caucasian counterparts, though there are very scanty data to verify this claim. There is thus an urgent need to launch an intense study of endometriosis in Black African women with a view to early diagnosis, especially among teenagers presenting with dysmenorrhea. This would also assist clinicians in sub-Saharan Africa to be conversant with relevant questions to ask when clerking a woman who presents with symptoms of endometriosis and to arrive at an accurate diagnosis, or a differential diagnosis of the disease.
History taking from women (or teenagers) with suspected endometriosis in African setting: relevant questions to ask and probe into:
A patient with endometriosis will not walk into a clinician’s consulting room and say “Doctor, I have endometriosis.” After the normal familiarization and “getting to know you”, the clinician should ask “What can I do for you” or “Why did you come to the clinic today?” The Nurses, the first point of call for the patient must have taken the necessary data such as her age, marital status, parity, blood pressure, pulse, temperature and breathing rate as well as height (in meters) and weight (in kilograms) for the calculation of the patients Body Mass Index. The age and occupation of the patient are also vital information to be recorded on her medical record file. Many clinicians forget these very simple steps which lead to misdiagnosis of endometriosis as will be seen later. Pain, in one form or another, at a particular location or another, especially in their girdle or pelvic pain is what brings her to the Doctor, though a significant proportion of patients with endometriosis remain asymptomatic.17 The Clinician is expected to probe further into the severity of the pain, the exact location of the pain (inguinal pain, lower abdominal pain, lower back pain, deep pelvic pain etc) and activity being carried out when the pain begins and what relieves the pain. Other important questions on pain may lead the clinician to a presumptive diagnosis of endometriosis. One particular pain the doctor should ask for is pain during intercourse or dyspareunia, which is commonly pathogneumonic of endometriosis. Another particular type of pain the doctor should ask for is dysmenorrhea or painful menstruation. Davila et al.,18 observed that dysmenorrhea usually precedes flow by a few days and begins to lessen 1-2 days into the menses. After noting the key point that brought the patient to the clinic, antecedents events are then probed for. It serves the clinician well to be systematic in her/his approach of the patient and should be patient-oriented. The formal enquiry should begin with her menstrual history. This should include
- 1. Age at menarche
- 2. Duration of monthly menses
- 3. Cycle length
- 4. Pain during menses (dysmenorrhea)
- 5. Prolonged and heavy bleeding during menses (menorrhagia)
and other pertinent questions relating to her menstruation and cycle. It may be appropriate here to ask for monthly cyclic bleeding elsewhere in her body or if she knows of any close relative (first-degree) that bleeds monthly elsewhere in her body. Davila et al.,18 is also of the opinion that a familial/genetic susceptibility to endometriosis has been documented, that a woman with a first-degree relative with endometriosis has a lifetime risk of the disease approximately 10 times that of a woman without an affected family member.
Female infertility and endometriosis
Literature is rife with data on the association of endometriosis and infertility.19-23 A study reported that between 30-50% of women diagnosed with endometriosis are also challenged with infertility while 25-50% of infertile women as well present with endometriosis and that Caucasian women more than African-American women are likely more prone to have endometriosis.24 According to WHO, endometriosis can be a risk factor for infertility consequent upon the presumptive outcomes of the disease on the pelvic organs such as ovaries, Fallopian tubes, uterus and the pelvic cavity.25 Clinicians and gynecologists in Africa should inquire about parity from women of reproductive age who present with pelvic pain. They should document primary or secondary infertility in such patients. Their fertility status, in addition to other symptoms, may consolidate the diagnosis of endometriosis.
Menstrual History toward diagnosis of endometriosis
The World Health Organization stated that a detailed and elaborate history of menstrual symptoms and chronic pelvic pain should furnish the basis for suspecting endometriosis.25 Ashrafi et al.,26 divided the symptoms of endometriosis into early and late stages, documenting gravidity, parity, family history of endometriosis, history of galactorrhea, previous pelvic surgery and shorter menstrual cycle length as risk factors for early endometriosis but not natural menstruation and age at menarche. The authors also related fatigue, diarrhea, constipation, dysmenorrhea, dyspareunia, pelvic pain and premenstrual spotting as being more discernible in late-stage endometriosis. African clinicians should painstakingly document menstrual history of their patients and have at the back of their minds that family history of endometriosis, dysmenorrhea, dyspareunia (in women in reproductive age group) and premenstrual spotting may consolidate the diagnosis of endometriosis.
Age, age at menarche and endometriosis
Women with endometriosis are usually in their reproductive age27-29 though the symptoms may have started during their teenage years into their third decade of life when they are between 20 and 30 years old. Most Black African women get married at this time and some of those who had been having symptoms of endometriosis find out that they may not be able to easily get pregnant. Staal et al.,30 noted that in Netherlands, delayed diagnosis of endometriosis is significantly increased in teenagers, and very frequently, the first signs of endometriosis commence in teenagers shortly after the menarche. Anecdotal report indicates that, in African setting, dysmenorrhea among teenagers is usually taken as normal menstrual pain and this has dire consequences that are yet to be reported on. Some studies have linked early age at menarche to endometriosis31 though this topic is still contentious and debatable. However, African doctors should inquire about and document age at menarche of their patient presenting with pelvic pain and infertility.
Duration of menstrual period and endometriosis
Duration of monthly menstrual period may be related to endometriosis. Vercellini et al reported slightly longer menstrual flow duration in women with endometriosis compared to those without endometriosis32 a notion supported by Treolar et al that shorter menstrual cycle length was not associated with endometriosis.33 Although more studies are needed to verify this assertion, however, a positive history of longer duration of monthly menstruation may strengthen the diagnosis of endometriosis in indigenous Black African women. African gynecologists and clinicians should be aware of this.
Cycle length and endometriosis (who wrote about this and what did they say)
In the study of Shafrir et al,.34 short menstrual cycle length was characteristically associated with endometriosis, a report that confirms what Missmer et al,.35 documented. Taking a cue from such studies, African doctors should inquire about cycle length from their patients for an additional evidence and better management of endometriosis and pelvic pain, if the cycle length of their patients is said to be shorter than normal.
Body Mass Index and endometriosis (who wrote about this and what did they say)
Many studies have conclude that there is an association between Body Mass Index (BMI) and endometriosis. For example, Ferrero et al,.36 reported that women with endometriosis have lower BMI and are less frequently obese than control subjects. Liu and Zhang37 concluded that higher body mass index may be associated with lower risk of endometriosis. Holdsworth and Carson38 expatiate further by declaring an reverse relationship between endometriosis and a BMI in a woman, though “the precise mechanisms and aetiological basis linking body mass index with endometriosis remain unknown.”
This paper has surveyed clinical diagnosis of endometriosis mostly in the developed world with very few references in sub-Saharan Africa. The diagnosis of endometriosis is not often made by African gynecologists and clinicians among Black African women with the illness. This may be due to lack of or inadequate training, minimal exposure and/or not being aware of the symptoms of the disease. Clinical presentations of endometriosis in Black African women may not be different from presentations among Caucasian women. Though a confusing illness for the patient and for the clinician, at least, African doctors can have a suspicion of endometriosis when a Black African woman presents with a combination of infertility, pelvic pain, dysmenorrhea and dyspareunia. As is often said, some patients may not present with any symptoms, but this may be at the initial stage of the disease but some tell-tale signs of endometriosis, which the clinician and the gynecologist should be aware of include age of the patient being in 2nd, 3rd or 4th decade of life, early age at menarche of 11 years and below, longer duration of monthly menstrual flow, probably shorter menstrual cycle and low Body Mass Index.
When African clinicians keep these points, specifically, robust menstrual history and Body Mass Index, in mind when a woman in reproductive age consults, definitely many women who suffer in silence or who are confused or unsure of what ails them can have relief and an answer to their health problem. This will also allow early diagnosis of endometriosis in Black African women, reduce number of consultations at different clinics, number of diagnosis or misdiagnosis and also minimize the amount of out-of-pocket expenditure as well as increase the quality of life of women with endometriosis. In addition, the true prevalence of the disease can be asserted in due course of time which may lend hand to possible better intervention and policy making by decision makers.
This paper recommends that the Federal Government, International Agencies such as United Nations Women Development, WHO, World Bank and UNDP as well as Philanthropists, should fund series of studies on endometriosis, starting from studies of dysmenorrhea among secondary school girls in Nigeria and other countries in Africa, and following these girls up for 5 or even 10 years for any development of endometriosis. Further, organizations such as Endometriosis Support Group of Nigeria should establish an electronic data base for all the patients who have been confirmed with endometriosis, liaise with other such organizations not only in Africa but in Europe, the Americas, Asia and Oceania and participate in annual conferences to share fresh ideas on all areas of endometriosis to bring about early and appropriate diagnosis and prompt and effective management of the disease.
None.
None.
No conflict of interest.
- 1. Kennedy S, Bergqvist A, Chapron C, et al. ESHRE guideline on the diagnosis and management of endometriosis. Hum Reprod. 2005;20(10):2698–704.
- 2. http://endometriosis.org
- 3. Guidice LC, Kao LC. Endometriosis. Lancet. 2004;364 (9447):1789–1799.
- 4. Vinatier D, Orazi G, Cosson M, et al. Theories of endometriosis. Eur J Obstet Gynecol Reprod Biol. 2001;96:21–34.
- 5. Vercellini P, Fedele L, Aimi G, et al. Association between endometriosis stage, lesion type, patient characteristics and severity of pelvic pain symptoms: a multivariate analysis of over 1000 patients. Hum Reprod. 2007;22:266–271.
- 6. Abrao MS, Podgaec S, Dias JA Jr, et al. Deep infiltrating endometriosis affecting the rectum and lymph nodes. Fertil Steril. 2006;86:543–547.
- 7. Podgaec S, Goncalves MO, Klajner S, et al. Epigastric pain relating to menses can be a symptom of bowel endometriosis. Sao Paulo Med J. 2008;126:242–244.
- 8. Arruda MS, Petta CA, Abrao MS, et al. Time elapsed from the onset of symptoms to diagnosis of endometriosis in a cohort study of Brazilian women. Human Reprod. 2003;18:756–759.
- 9. Kennedy S, Bergqvist A, Chapron C, et al. ESHRE Special Interest Group for Endometriosis and Endometrium Guideline Development Group, ESHRE guideline for the diagnosis and treatment of endometriosis. Human Reproduction. 2005;20(10):2698–2704.
- 10. Galle PC. Clinical presentation and diagnosis of endometriosis. Obstet Gynecol Clin North Am. 1989;16(1):29–42.
- 11. Spaczynski RZ, Duleba AJ. Diagnosis of endometriosis. Semin Reprod Med. 2003;21(2):193–208.
- 12. Agarwal SK, Charon C, Guidice LC, et al. Clinical diagnosis of endometriosis: a call to action. American Journal of Obsterics and Gynecology. 2019;20(4):354.e1–354.e12.
- 13. Kyama CM, Mwenda M, Machoki J, et al. Endometriosis in African Women’s Health. 2007;3(5):629–635.
- 14. Maillard C, Cherif Alami Z, Squifflet JL, et al. Diagnosis and Treatment of Vulvo-Perineal Endometriosis: A Systematic Review. Front Surg. 2021;8:637180.
- 15. Byanyima RK. Menstruation in an unusual place: a case of thoracic endometriosis in Kampala, Uganda. Afr Health Sci. 2001;1(2):97–98.
- 16. Ajayi AB, Ajayi VD, Biobaku O, et al. A 10-year study of endometriosis in an indigenous black African population. Journal of Endometriosis and Pelvic Pain Disorders. 2016;8(4):157–166.
- 17. Buchweitz O, Poel T, Diedrich K, et al. The diagnostic dilemma of minimal and mild endometriosis under routine conditions. J Am Assoc Gynecol Laparosc. 2003;10(1):85–89.
- 18.Davila GW, Kapoor D, Alderman E, et al. Endometriosis Clinical Presentation. Medscape Reference.
- 19. Somigliana E, Vigano P, Benaglia L, et al. Management of Endometriosis in the Infertile Patient. Semin Reprod Med. 2017;35(1):31–37.
- 20. Soriano D, Adler I, Bouaziz J, et al. Fertility outcome of laparoscopic treatment in patients with severe endometriosis and repeated in vitro fertilization failures. Fertil Steril. 2016;106(5):1264–1269.
- 21. Macer ML, Taylor HS. Endometriosis and infertility: a review of the pathogenesis and treatment of endometriosis-associated infertility. Obstet Gynecol Clin North Am. 2012;39(4):535–549.
- 22. Practice Committee of the American Society for Reproductive Medicine. Endometriosis and infertility. Fertil Steril. 2006;86(5 Suppl 1):S156–S160.
- 23. Adamson GD. A 36-year-old woman with endometriosis, pelvic pain, and infertility. JAMA. 1999;282(24):2347–2354.
- 24. Evans MB, Decherney AH. Fertility and Endometriosis. Clin Obstet Gynecol. 2017;60(3):497–502.
- 25. http://www.who.int/news-room/fact-sheets/detail/endometriosis.
- 26. Ashrafi M, Sadatmahalleh SJ, Akhoond MR, et al. Evaluation of Risk Factors Associated with Endometriosis in Infertile Women. Int J Fertil Steril. 2016;10(1):11–21.
- 27. Broi MGD, Ferriani RA, Navarro PA. Ethiopathogenic mechanisms of endometriosis-related infertility. JBRA Assist Reprod. 2019;23(3):273–280.
- 28. Della Corte L, Di Filippo C, Gabrielli O, et al. The Burden of Endometriosis on Women's Lifespan: A Narrative Overview on Quality of Life and Psychosocial Wellbeing. Int J Environ Res Public Health. 2020;17(13):4683.
- 29. Culley L, Law C, Hudson N, et al. The social and psychological impact of endometriosis on women's lives: a critical narrative review. Hum Reprod Update. 2013;19(6):625–639.
- 30. Staal AH, van der Zanden M, Nap AW. Diagnostic delay of endometriosis in the Netherlands. Gynecol Obstet Invest. 2016;81:321–324.
- 31. Nnoaham KE, Webster P, Kumbang J, et al. Is early age at menarche a risk factor for endometriosis? A systematic review and meta-analysis of case-control studies. Fertil Steril. 2012;98(3):702–712.e6.
- 32. Vercellini P, De Giorgi O, Aimi G, et al. Menstrual characteristics in women with and without endometriosis. Obstet Gynecol. 1997;90(2):264–268.
- 33. Treloar SA, Bell TA, Nagle CM, et al. Early menstrual characteristics associated with subsequent diagnosis of endometriosis. Am J Obstet Gynecol. 2010;202(6):534.e1–6.
- 34. Shafrir AL, Farland LV, Shah DK, et al. Risk for and consequences of endometriosis: A critical epidemiologic review. Best Pract Res Clin Obstet Gynaecol. 2018;51:1–15.
- 35. Missmer SA, Hankinson SE, Spiegelman D, et al. Reproductive history and endometriosis among premenopausal women. Obstet Gynecol. 2004;104(5 Pt 1): 965–974.
- 36. Ferrero S, Anserini P, Remorgida V, et al. Body mass index in endometriosis. Eur J Obstet Gynecol Reprod Biol. 2005;121(1):94–98.
- 37. Liu Y, Zhang W. Association between body mass index and endometriosis risk: a meta-analysis. Oncotarget. 2017;8(29):46928–46936.
- 38. Holdsworth-Carson SJ, Rogers PAW. The complex relationship between body mass index and endometriosis. Journal of Endometriosis and Pelvic Pain Disorders. 2018;10(4):187–189.

