Non-Caucasian patients from the Middle East, North Africa, India, East Asia, Latin America, and the Persian region are known to present particular problems to the rhinoplasty surgeon. These patients' skin is heavier and thicker, the alar cartilages are softer and wider, the tip is usually poorly defined, the columella is short, and the process of wound contracture and scaring is unpredictable, involving more fibrosis. Unless a good technique has been used for tip refinement, the results will be disappointing and the tip will become ptotic after surgery, resulting in Under projection, Polly beak, wider nares, collapse, and even deviation. Therefore, a properly applied tip-refinement technique will avoid these undesirable problems and achieve adequate tip projection, definition, refinement, rotation, and symmetry. In addition, the rhinoplasty surgeon should take into consideration the patient's ethnic origin as well as local, social, and traditional manners.
"Rhinoplasty appears to be an easy operation, but it is hard to produce consistently good results," stated Gustave Aufricht.1 The author supports this statement, even skilled rhinoplasty surgeons are never sure how the nose will finally heal because healing is subject not only to the most predictable technique but also to unpredictable and uncontrollable wound contracture, fibrosis, and scaring.2 Consequently, the surgeon must consider supportive means in order to compensate for the loss of tip support and to avoid the unpleasant postoperative effects of the ptotic tip.3-5 Resulting in Under projection, drooping, hanging columella, Polly beak, acute nasolabial angle, or wider nares.6
This review article is based on the author’s over thirty years experience on rhinoplasty. The author’s practice has been limited to rhinoplasty and facial plastic surgery since 1993. The author performed over twenty thousand rhinoplasties on patients of multiethnic origin, during his practice in cosmopolitan cities (London, Jeddah, Dubai). Also, the author wrote a textbook on rhinoplasty & facial plastic surgery, was published in 2002 (500 pages/over 1000 illustrations - www.rhinoplastybizrahacademy.com).
Keywords: Rhinoplasty, Facial plastic surgery, Non caucasian patients
For non-Caucasian patients, the following factors must be taken into consideration:
1. The thickness of the investing skin: thicker skin is the least likely to achieve desirable refinement and definition. Thicker skin may fail to contract favorably on the newly reshaped cartilages and lead to excessive soft tissue scarring. There needs to be enough subcutaneous tissue to provide adequate cushioning over the nasal skeleton, yet still allow critical definition of the nasal tip.7 Also, thick skin creates the heavier tip that become heavier with postoperative oedema predisposing for the ptotic tip.
2. The strength and contour of the alar cartilages: the alar cartilages are softer, wider, and shorter, with obtuse domal angles and ill-defined intermediate crus.
3. Wound healing and contracture: the healing process in patients with Fitzpatrick skin types III, IV, and V involves more scaring and fibrosis, because of increased population of the fibroblast cells as we move down Fitzpatrick list. Therefore, there is more wound contracture and scaring that later presents uncontrolled problems such as Polly beak, notching and, to a lesser extent, pinching, dimpling, retractions, and even deviation when there is more wound contracture on one side than the other.
4. Heavy tip: Caucasians generally have thin skin with strong cartilage, whereas Arabs, Indians, Asians, and Africans have relatively thicker skin, more subcutaneous fatty fibrous tissues, and softer cartilages. This anatomy increases the anatomic weight of the tip, which is doubled or tripled in the weeks following surgery due to edema. After the absorption of the sutures, the tip will drop down due to the effects of gravity, with an increase in septocolumellar redundant soft tissue.
-
5. Patient misconduct: some patients may not adhere to postoperative instructions. It is common for patients to prematurely remove the cast at home as they are curious to see the results of the surgery. Furthermore, when attempting to clean blood clots, they may inadvertently pull-down stitches of the marginal incision, which may cause lateral crus collapse. Other reasons include sun exposure, early wearing of glasses, practicing sports, exposure to trauma (pai1icularly that caused by their children), or forgetting their postoperative antibiotics, leading to infection.8
To understand the effects of routine rhinoplasty incisions and excisions, in both open and closed approaches the surgeon should be aware of the anatomic factors that maintain tip support:6
- Medial crura attachment to the caudal septum
- Attachment of upper and lower lateral cartilages to each other
- Ligamentous attachment of anterior septal angle to the dome
- Length and direction of lateral crura (in the non-Caucasian nose, the lateral crus is commonly long and drooped)
- The dorsal septum, caudal septum, the lower and the upper lateral cartilages
These ligaments and attachments are more lax, soft, and fatty in the non-Caucasian nose compared with the Caucasian nose, which predisposes loss of tip support following surgery.
1. Routine rhinoplasty incision and excision in open or closed approach: the Intercartilaginous and transfixion incisions, caudal septum exposure with cephalic trimming of the lateral crura will divide most anatomic attachments, predisposing to loss of tip support (Under projection; dropped bulbous tip; short, retracted, or hanging columella; Polly beak; acute nasolabial angle; and increased alar flare).
2. Tip-supportive means during surgery have not been considered: the use of the techniques of new double dome creation, scoring, suture fixation, columellar strut (as indicated in this article); tip graft, and septocolumellar sutures are highly recommended in non-Caucasian patients in order to achieve adequate tip projection, support, definition, and rotation.
3. Hypertonic depressor septi nasi muscle: strong nasolabial muscle pulls the nose down while laughing, chewing, or even during talking. In these cases, division of the nasolabial muscle through sublabial incision will increase rotation and reduce the tension on the tip.
4. The use of septocolumellar sutures alone in efforts to achieve the desired tip profile is inadequate. One must consider tip refinement and supportive means.
5. Excessive trimming of caudal septum, lateral crus, nasal spine, and cartilaginous hump.
- 6. Transfixion incision or caudal septum exposure has been extended too far down, dividing the attachment between nasal spine and base of the columella.
7. Open approach is non-exempt, also divide most anatomical attachments, almost all anatomical attachments are divided in open approach, during exposing the caudal septum, the interdomal spaces, lateral crus and cephalic lateral crus trimming. Therefore, open approach is not that much advantage on closed approach as most surgeons think.
- The tip may be poorly defined, wide, with varying degrees of bulbosity (trapezoid, boxy), bifid, round, under projected, and/or drooping. Depending on ethnic origin.
- Thicker and heavier skin with subcutaneous fat
- Short, bifid, hanging, or retracted columella
- Underdeveloped anterior septal angle and short caudal septum
- Large upper lateral cartilages with curved or bent caudal ends (Mediterranean).
- High bony compartments
- Low bony compartments (African, East Asian)
Joseph's methods cannot, of course, be abandoned altogether because most of his technical steps are involved in every rhinoplasty performed. To avoid unpleasant effects of the dropped tip, the blind Intercartilaginous excision of the lateral crus must be avoided and additional maneuvers during the procedure must be considered to obtain more tip projection, refinement, definition, and symmetry. The concept of Goldman's tip is still the basis of the newly developed, more predictable additional tip maneuvers of new double dome creation, scoring, and suture fixation. These maneuvers have been reinforced by the use of columellar strut and Sheen tip grafts.2,9 Regarding open or closed, delivery approaches, in short, a strong tripod of conjoined lateral-to-medial crura supported by the columellar strut and tip graft is achieved.10 In this way, the possibility of alar notching, alar collapse, pinched nasal tip, and asymmetry are reduced to a minimum of 5% to 15%. These untoward results are due to the effect of wound contraction and the healing process along the exposed lateral crus and the marginal incisions rather than being due to technical faults. The author recommends the following maneuvers Figure 1, These maneuvers can be performed by closed or open approach. It is not important how you go in; what important is what you do when you are ‘in’:
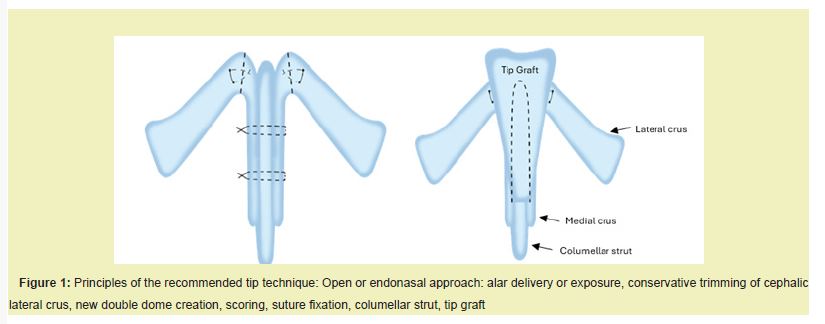
- 1) Approach: a) Open approach via a mid-columellar incision
- 2) Septoplasty or obtaining septal graft.
- 3) Tip-refinement technique.
- a) Alar delivery and cephalic trim of lateral crus with preservation of at least 8mm of vertical lateral crus
- b) New double dome creation, scoring, and suture fixation
- c) Columellar strut: Long strip or triangular extended graft
- d) Tip graft: Long, short or shield graft.
- e) Lateral crura overlay technique is indicated in order to reduce the volume of the lateral crus, as in flared lateral crura, over projection and in drooping tip.
- 4) Conservative hump removal
- 5) Osteotomies: lateral, medial and, as indicated intermediate and transverse in crooked noses.
- 6) Supratip and dorsum augmentation, as indicated in saddling.
- 7) Alar base resection, as indicated.
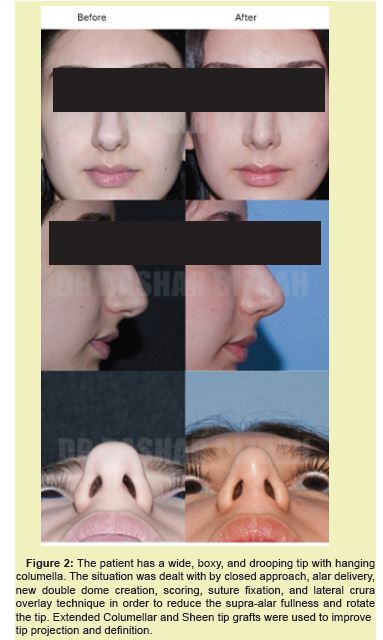
b) Endonasal approach with Intercartilaginous and marginal incisions
The first attempts to improve tip projection were made by Irving Goldman.11 Goldman's tip was based on cutting the angle between the medial and lateral crura and suturing the medial crura together. Safian12 (Joseph student) vertically cut the dome, but Goldman's concept was that the more lateral cut would augment the medial crura and, thus, improve tip projection.13 Although Goldman's tip was a creative technique, in time, surgeons realized its problems of pinching, notching, retraction, asymmetry, and pointed tip. The concept of Goldman's tip has been modified and developed further by master rhinoplasty surgeons of the past 40 years (Sheen, Simon, McCollough, Tardy, Kridel, Toriumi, and Peck and others) who developed techniques of new double dome creation through scoring, suture fixation, columellar strut, and tip graft. The objective is to obtain a clearly defined and properly projecting tip that appears symmetric and triangular on basal view and that flows and blends well with the rest of the nose. In the author's series of massive number of rhinoplasties performed on people from the Middle East, the Gulf, Asian and North Africa, it has been found that the maneuvers of new double dome creation that utilize scoring, suture fixation, columellar strut and, as indicated, tip grafts are a key to successful rhinoplasty. These maneuvers achieve adequate tip projection, elevation, definition, refinement, rotation, and symmetry, with the least and most easily managed postoperative problems Figure 2.
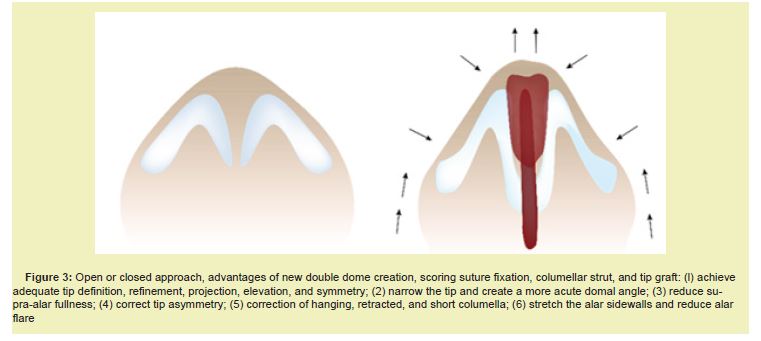
Tip projection, definition, minimal elevation, rotation, and narrowing are achieved by increasing the length of medial crura and shortening the lateral crura (new double dome creation). Scoring or oblique dome division creates a more acute domal angle for tip definition. Suture fixation of the medial crura to the lateral crura at the dome creates a more acute domal angle and establishes a totally new double dome.2 It provides additional tip definition, refinement, and narrowing, and a minimal degree of tip projection. Also, it stretches the alar sidewalls and reduces alar flare. Excision of the cephalic-based triangle at the dome and suture fixation will achieve more tip narrowing and supra-alar definition Figure 3.
The aim is to preserve the integrity and continuity of the anatomic natural tripod structures of the medial and lateral crura that are bound together by simple or mattress sutures at the newly created double dome to achieve a more favorable acute domal angle for pleasant tip definition and refinement.
More tip projection and definition are achieved by the use of a columellar strut and as indicated, a crushed shield tip graft.9 The columellar strut and tip graft will reinforce and strengthen the medial crura and the dome in the already-achieved tripod structures of bound medial and lateral crura, thus creating a strong, supported, projected, and well-defined tip. All above mentioned maneuvers can be performed by open, closed or delivery approach.
The author usually uses the endonasal approach of Intercartilaginous and marginal incisions and performs alar delivery. A tissue forceps is then pushed under the bilaterally delivered alar cartilages in order to obtain elevation and symmetry and to create a new, more acute domal junction between the medial and lateral crura (apex of the dome). This maneuver will lengthen the medial crura and shorten slightly the lateral crura, which is essential for tip projection and symmetry see Figures 1-3.
New double dome creation, scoring and suture fixation
The newly created double dome at the apex is now scored vertically on each side, preserving the vestibular skin and mucosa. A 4/0 polydioxanone (PDS) interdomal buried suture is passed posteriorly through the intermediate and lateral crura 1 mm below the scored area in a simple or mattress suture in order to create a more acute domal angle and preserve a stable tripod structure of the conjoined lateral and medial crura. The mattress suture fixation will convert the convex lateral crura to a concave lateral crura, reducing the supra-alar fullness. The advantages of new double dome creation, scoring, and suture fixations are: -
- 1. To create a more acute domal angle between the lateral and medial crura, resulting in a more defined triangular tip see figure 3.
- 2. To achieve more tip definition and refinement.
- 3. To narrow the tip and domal arch.
- 4. To reduce supra-alar fullness and convert a convex lateral crura to a concave crura.
- 5. To increase projection.
Columellar strut
A precise pocket is dissected between the two medial crura. This pocket should extend to a depth of approximately 2 mm above the nasal spine. Mattress sutures are used to fix the strut (septal or conchal) that lies between the two medial crura. The columellar strut is indicated in order to obtain the following: increased tip projection, definition, and refinement; preservation of tip projection; correction of hanging columella; correction of buckled medial crura; correction of retracted columella; correction of tip asymmetry; strengthening weak medial crura; a stable site for tip grafting; and the correction of bifid columella see Figure 1.
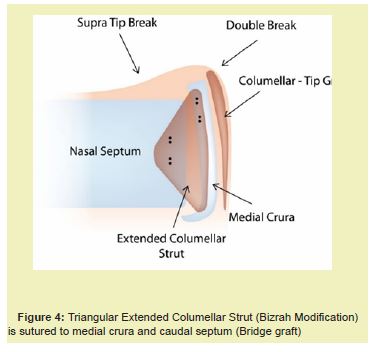
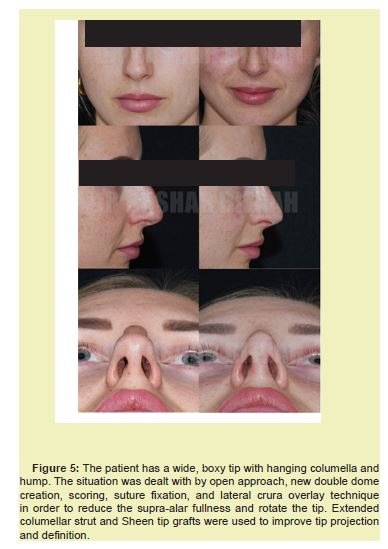
Extended columellar strut
The new advances of the modified Bizrah Triangular Extended Columellar strut has promoted the outcome of Tip Plasty. The Triangular Extended Columellar Strut (3cm x 1.5cm) will bridge between the medial crura and the caudal septum, this will obtain more stable and fixed-in tip, also will obtain more tip projection, elevation, and rotation Figure 4,5. this will significantly reduce the ptotic tip after surgery and reduce the tip down movements during laughing and talking.
Tip graft
The wide leading edge of the tip graft is rounded and beveled to avoid sharp edges and demarcation of the skin. In thin-skinned patients, the graft is crushed or softened with a crusher in order to prevent showing through the skin. The tip graft is positioned at the level of the dome.14 Usually four (4/0 Vicryl-Beige Braided Polyglycolic Acid) are used. The tip graft is sutured to the caudal margin of the medial crura. Indications for tip graft are Improved. tip definition projection, refinement, and contouring; creation of a well-defined double break; creation of a well-defined supra-tip break; and a nicely contoured infratip lobule. A long graft narrows the tip and increases tip projection; corrects dome asymmetry and tip bifidity; increases rotation of the dome and tip; supports the columella in the retracted columella, weak medial crura, hanging columella, and bifid columella; and augments the acute nasolabial angle. Double grafts are used to achieve more tip projection, definition, and refinement in a very thick-skinned patient and to increase the length of the over-rotated nose by increasing the distance from the nasal starting point (the nasion) to the tip-defining points (infratip lobule) see Figure 1.
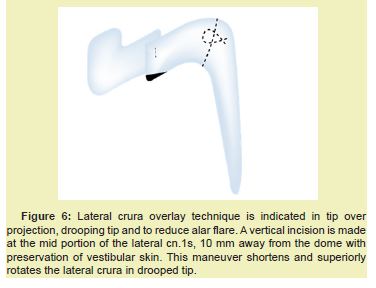
Lateral crura overlay technique
This technique is reserved for more difficult tips when the volume of the lateral crura needs to be reduced, such as: -
- Drooping Tip: In order to reduce the length of the lateral crus.
- Broad & Boxy Tip: In order to break lateral crus convexity to reduce the Supra-Alar fullness without over reduction of lateral crus.
- Over projected Tip: In order to reduce the length of both lateral and medial crura.
- Asymmetry Tip: In order to obtain more tip symmetry by shortening the longer lateral crus.
The technique described by Kridel and Konior15 and Webster and Smith16 produces a more natural appearance, without excessive cartilage excision. Open or closed, delivery approach, following the maneuvers (new double dome creation, scoring, suture fixation, columellar strut and, as indicated, tip graft), the lateral crura is inspected. A straight vertical incision is then made at the middle portion of the lateral crura, at least 10 mm away from the dome. The incision is located midway between the dome and free posterior margin of the lateral crus, with the preservation of the skin vestibule. The cartilage is then undermined above the vestibular skin toward the dome for 2 mm to 5 mm, according to the required correction of shortening or rotation. The free undermined crura segment will overlay the posterior segment, resulting in shortening of the lateral crura, with preservation of the lateral crus cartilage. After the optimal tip position is determined, a vertical mattress suture is placed on the overlayed cartilage. This suture firmly locks the tip into the desired position. If rotation is required, excessive cartilage in the form of a triangle develops along the caudal crural margin. This cartilage should be trimmed in order to achieve a straight alar rim. The marginal incision is then sutured with 4/0 Vicryl Figure 6. The same technique can be applied on the medial crura in overprojected tips in order to lower the tip.
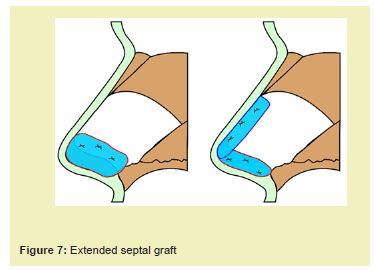
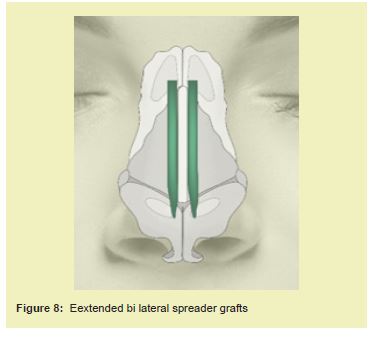
Short nose
The extended septal graft is the most important key maneuver to consider in order to lengthen the nose Figure 7. Also, extended bilateral spreader grafts may be considered in order to push the tip inferiorly and lengthen the nose. Figure 8. The extended septal graft is different from the Bizrah Extended columellar strut Figure 4, The purpose of extended septal graft is to extend the caudal septum and lengthen the nose, while the extended columellar strut Figure 4 purpose is to obtain more stable tip projection and rotation. However, both grafts will stabilize the tip to the septum and reduce possibility of ptotic tip following surgery.
Saddle nose
The correction of the saddle nose for people of African, East Asian origin and the saddling following severe trauma to the nose.
The correction of Saddle Nose key maneuvers are: -
1. Open or Endonasal approach.2. Obtain septal, conchal or rib graft. Also a synthetic grafts as indicated.
3. Full Tip Plasty maneuvers: New double dome creation, suture fixation, columellar strut, Tip graft and Later crus approximation suture.
4. Dorsal graft preparation:
- Shaping the graft to the required length and width.
- Suturing layered double or triple graft together.
- - Beveling, scoring and trimming of the edges to avoid showing through the skin and
skin step deformity - Positioning the graft in the exact site.
- Stabilizing the graft and suturing it to the dorsum septum or dome apex or the use of skin pullout suture. May be used to fix the graft cephalically.
5. Alar wedge excision: to reduce the flared rim and the wide nostril floor. Following tip elevation and projection, the flaring of the nostrils will have been reduced and if there's still excessive flaring of more than 3mm outside the medial canthal line, this can be corrected by alar base resections. The first incision follows the Alar’s natural crease but ends in the floor 2 to 3mm medial to the rim insertion. The second incision includes a few millimeters of the rim in a triangular wedge and meets the first incision laterally in a triangular fashion.
6. Dressing and cast application: Steri-strips are used to apply a gentle pressure in order to eliminate the dead space and keep the nasal tissue in direct contact with the graft, which is vital for the graft to survive. External splints are applied gently to keep the graft in the middle and for stability of the nose.
post operative technical problems are unlikely because these maneuvers create a profound, strong, and oriented tripod of the conjoined lateral-to-medial crura supported by columella and tip grafts. Usually, the problems encountered are related to the process of wound healing, contracture, and scarring along the alar sidewalls, such problems as mild notching, pinching, collapse, or nares asymmetry.17
Common problem solutions
- 1. Mild notching and pinching are usually treated by small pocket incision batten or rim grafts.
- 2. Nares asymmetry is treated by narrowing the wider side.
- 3. Tip deviation is treated by adjusting the columellar strut, tip graft, batten grafts on the weak alar side, or lateral crura overlay technique on the flared side.
- 4. Bony dorsum deviation is corrected by re-osteotomy under local anesthesia.
- 5. Dorsum collapse or depression is corrected by fill-in pocket grafts.
- 6. Pollybeak is corrected by excising the problem tissue (high dorsum septum or supra-tip scarred tissue) and tip elevation by septocolumellar suture.
- 7. Persistent hump: due to fibrosis on dorsum, corrected by gentle rasping and the use of Fascia-Lata to overcome roughness and irregularities on dorsum.
The factors maintaining tip symmetry are: -
- 1. Symmetric marginal incision
- 2. Symmetric alar delivery
- 3. Equal dome scoring
- 4. Accurate positioned mattress sutures at the dome
- 5. Length of columellar strut, which should be positioned above the nasal spine to avoid displacement and deviation.
- 6. Accurate positioning of the superior mattress suture that binds the bilateral intermediate crura to the columellar strut.
- 7. Accurate positioning of the midline tip graft
- 8. Lateral crura overlay technique for unilateral or bilateral flared lateral crura.
- 9. Accurate marginal incision closure.
The author does not recommend the following techniques in Non-Caucasian patients:
1. The classic reduction technique: the Joseph reduction rhinoplasty without considering tip supportive means is not recommended. It will almost definitely end with loss of tip suppo1t and the unpleasant result of dropped, broad bulbous tip; pollybeak; hanging or retracted columella; alar collapse; acute nasolabial angle; and increased alar-rim flaring. The Joseph technique, in the author's experience, should only be reserved for Caucasians or those patients with minor bulbosity or minor hump, strong cartilage, and adequate tip rotation and projection.
2. The classic Goldman procedure: this procedure results in many problems such as pinching, notching, alar retraction and collapse, poor tip definition and asymmetry, unwanted creases, nasal bossae, and pointed tip.13 All these problems are directly related to the division of the lateral crura with vestibular skin (disturbing the continuity of lateral crura) and to the domal sharp edges that have not been covered by shield tip grafts.
3. Suturing techniques: some surgeons try to achieve the desired tip profile in relation to dorsal profile by septocolumellar sutures only, suturing the trimmed caudal septum to the pulled up medial crura to achieve rotation and projection. In the author's opinion, this is a misleading maneuver and gives false impressions. A few weeks later, the suture will be absorbed, and the tip, which is not being supported by grafts, will drop down again. This suturing technique should only be used to achieve more rotation in patients with an already-adequate tip definition, projection, refinement, and strong alar cartilage but should not be used in Non-Caucasian patients who have a relatively heavier tip. The author stresses that the desired dorsum and tip profile should have been achieved before the application of any septocolumellar sutures because this is how the nose is going to look after a few months. Sutures are only used to preserve and support the desired profile, not to achieve rotation and projection.
Oblique dome division / Preservation rhinoplasty (Bizrah modification)
Modified Oblique dome division without delivery of the lateral crus (Bizrah Technique). The reduction rhinoplasty, as indicated, has many unpleasant effects: dropped tip, pollybeak, asymmetry, alar collapse, hanging columella, and wider nares. The Goldman technique has also resulted in problems such as pinching, notching, retraction, asymmetry, alar collapse, and pointed tip. The author, however, highly recommends (as described) the technique of new double dome creation, scoring, suture fixation, columellar strut, and tip grafts. It has the most predictable results because it preserves the continuity of the lateral crus and obtains a strong tripod of conjoined lateral-to-medial crura supported by columellar and tip grafts, thus reducing very much the possibility of asymmetry, alar collapse, dropped tip, pinching, notching, and alar retraction. Because of the lateral crus marginal incision, lateral crus delivery and exposure, however, there may be unavoidable minor problems due to wound healing and contracture along the side walls, such as mild notching, pinching, and dimpling. To avoid even these minor problems, the author has developed a new technique that is largely based on the Goldman tip and the I-beam of medial crura but without lateral crus delivery (the Bizrah Modification).3 This technique keeps an intact alar rim and avoids any healing problems along the alar sidewalls such as dimpling, notching, retraction, collapse, or asymmetry. The author has performed this technique for over 25 years. In his opinion, this technique is very useful in achieving tip projection, definition, and refinement Figure 9 in the following situations: (I) tip underprojection; (2) short columella; (3) mild tip bulbosity; (4) in revision cases when lateral crus delivery is technically difficult; and (5) congenital pre-existing mild alar pinching and dimpling (in these situations, alar delivery will cause more deformity).
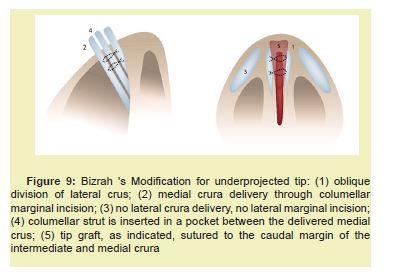
The principles are:
- Modified Oblique Dome Division
- Intermediate Crus Delivery and I-beam
- No Lateral Crus delivery
- No lateral crus marginal incision
- Creation of strong cartilaginous foundation in the midline of conjoined medial to intermediate crura supported by Columella strut and as needed additional Columellar-Tip graft.
- 1. Marking the tip defining point on both side of the tip (Highest point on the tip). And then mark it down on the alar rim, and then internally on the alar cartilage, this line will separate lateral crus from the intermediate crus.
- 2. Usually, procedure done with local anaesthesia with sedation.
- 3. An Endonasal approach and obtaining septal or conchal graft.
- 4. Marginal columella incision from mid-columella and up to the level of the external soft triangle at junction of intermediate to lateral crura. There is no marginal incision along the caudal margin of the lateral crura.
- 5. Modified Oblique dome division: The incision is now extended obliquely in the intermediate crus from medial to lateral. In a way to fully preserve the rim cartilage and divide the intermediate crura into the caudal portion (Rim cartilage) and a Cephalic portion (Never borrow or steal any portion of lateral crus).
- 6. The bilateral Cephalic portion of intermediate crura are delivered to one side.
- 7. A pocket is created between the medial crura down to nasal spine and caudally to expose the caudal septum, and a Triangular Extended Columellar Strut is now inserted and sutured (5/0 PDS) to both medial crura and Caudal septum. (Bridging between the medial crura and caudal septum). This will obtain a strong sustained tip projection, elevation and rotation.
- 8. An additional Tip-Columellar long graft is positioned and sutured to the caudal margin of the intermediate and medial crus. The grafts should be crushed and bevelled in order to avoid demarcation. The graft is long in order to augment the Naso-labial angle and obtain more rotation.
- 9. The re-oriented complex structure of medial and intermediate crura with columellar strut and the tip graft are pushed back inside the nose into a normal position. The transfixion and marginal incisions are closed with 5/0 PDS. Then additional two septocolumellar sutures are used to fix the medial crura/ columellar strut complex to the caudal septum.
- 10. Now under direct vision using sharp double-hook, only 1-2mm of cephalic lateral crus is trimmed, in order to reduce supra-alar fullness and allows a space for rotation.
- 11. Now, we already have established a very strong cartilaginous foundation in midline of conjoined medial crura to the intermediate crura, Extended triangular columellar strut, as needed additional columella and tip graft. Those are 6 strong structures in the midline in order to obtain adequate tip projection, symmetry, definition, refinement and rotation with full preservation of the integrity of the lateral crus (No marginal incision or delivery)
- 12. Special Inter-Lateral Crus Approximating suture for Wider Tips: The Lateral Crus Approximating Suture is extremely useful in almost 90% of the cases except patient with very thin skin. Using 5/0 PDS or 6/0 Proline, the suture is passed through superior septal angle from left to right, then through the cephalic lateral crus on the right side, then back through the cartilaginous dorsum portion 1mm behind SSA. Then passed through the left lateral crus cephalic margin, then knot the suture. It has a great advantageous: Reduce supra-alar fullness with more tip definition and refinement, stabilize the bi-lateral crus to the cartilaginous dorsum portion, stretch the alar sidewalls and reduce alar flares, stabilize the midline strong cartilaginous foundation (of the Medial crura, Intermediate lateral crus, Columellar strut and Tip graft) and increase tip rotation.
- 1. No lateral crus marginal incision and exposure: Preservation of the entire lateral crus on the alar sidewalls. Thus, reducing as much as possible alar retraction, notching, collapse, dimpling, asymmetry and even deviation.
- 2. The trimming of cephalic lateral crus is made more visible, more accurate and has better control.
- 3. Less postoperative oedema and crustation.
- 4. More natural looking alar sidewalls.
- 5. Stretches the alar sidewalls and reduces the alar flare.
- 6. Achieves adequate tip projection, elevation, definition, rotation and refinement.
- 7. Corrects Tip Bulbosity, Bifid tip, and Drooping tip, when combined with conservative retrograde cephalic trimming of the lateral crura (ten mm to be preserved) and combined with lateral crus approximating suture.
- 8. Corrects overprojecting tip. This is achieved by conservative trimming of the proximal ends of the lateral crura and superior ends of the intermediate crura. The author believes that lateral and medial crura overlay technique is best for correction of the overprojected tip as you will have direct control.
- 1. It should be performed in a very precise, accurate and symmetrical way.
Otherwise, unilateral, or bilateral alar collapse, pinching, notching or retraction might occur, which will require revision with Batten grafts. Anyone unwilling to work carefully to attain a stable symmetrical structure should not attempt this technique (Never borrow or steal any portion of lateral crus). - 2. Pinching: If you over-borrow from lateral crus, you will end with tip pinching. Therefore, do not borrow any portion of the lateral crus, preserve the rim cartilage and full integrity of the lateral crus.
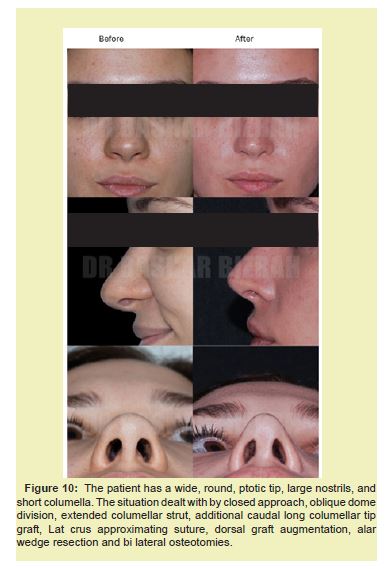
- 3. Although in Thin skin patients, may develop mild tip pinching, therefore avoid lateral crus approximating suture in very thin skin patient Figure 10.17-21
Advantages of Oblique Dome Division
Disadvantages of oblique dome division
This review article is based on the author’s over thirty years experience. Hopefully, we covered most of the key maneuvers which are required for a satisfactory and long-lasting outcome. Gustave Aufricht stated, “Rhinoplasty appears to be an easy operation, but it is hard to produce consistently a good result”. Actually, no respectful surgeon would guarantee rhinoplasty results, because our results are influenced and controlled by the thickness and nature of the investing skin, the strength and contour of the alar cartilages and unpredictable and uncontrolled nature of wound contracture, scarring and fibrosis along the alar side walls and dorsum. Therefore, preserved, balanced maneuvers of reduction, augmentation and tip supportive means form the basis of the direction which rhinoplasty is currently heading.
None.
This Review Article received no external funding.
Regarding the publication of this article, the author declares that he has no conflict of interest.
- 1. Aufricht G. The Development of Plastic Surgery in the United States. Plast Reconstr Surg. 1946;1:3.
- 2. McCollough EG. Surgery of the nasal tip. Otolaryngol Clin North Am. 1987;20(4):769-784.
- 3. Bizrah MB. Modified vertical dome division without delivery of the lateral crus. Arch Facial Plast Surg. 2002;4(3):198-199.
- 4. Tardy ME, Toriumi DML. Alar retraction: composite graft correction. Facial Plast Surg. 1989;6:101.
- 5. Sheen JH. Achieving nasal tip projection by the use of a small autogenous vomer or septal cartilage graft. Plast Reconstr Surg. 1975;56:35-40.
- 6. Toriumi D, Johnson C. Revision rhinoplasty. Aesthetic Facial Surg. 1991;2:411-456.
- 7. Flowers RS. The surgical connection of the non-Caucasian nose. Clin Plast Surg. 1977;4:69-87.
- 8. Bizrah MB. Rhinoplasty. Pioneer Cosmo Group. 2001.
- 9. Sheen JH. The Sheen tip graft. St. Louis: Quality Medical Publishers. 1991.
- 10. Toriumi DM, Johnson Jr CM. The crooked nose. Oper Tech Otolaryngol-Head Neck Surg. 1990;1:252-254.
- 11. Goldman IB. New technique for corrective surgery of the nasal tip. Arch Otolaryngol. 1953;58:183-218.
- 12. Safian J. The split cartilage tip technique of rhinoplasty. Plast Reconstr Surg. 1970;45:217.
- 13. Simons RL, Fine IJ. Evaluation of the Goldman tip in rhinoplasty. In: Proceedings of the Second international Symposium on Plastic and Reconstructive Surgery of the Face and Neck. New York: Grune & Stratton. 1977:pp.39-46.
- 14. Sheen JH. Aesthetic rhinoplasty. St. Louis: C.V. Mos. 1978.
- 15. Kridel RWH, Konior RJ. Controlled nasal tip rotation via the lateral crura overlay technique. Arch Otolaryngol Head Neck Surg. 1991;117:411-415.
- 16. Webster RC, Smith RC. Lateral crural retrodisplacement for superior rotation of the tip in rhinoplasty. Aesthetic Plast Surg. 1979;3:65-78.
- 17. Bull TR, Mackay IS. Alar collapse. Facial Plast Surg. 1986;3:268.
- 18. Toriumi DM, Russel RM. Innovative surgical management of the crooked nose. Facial Plast Surg Clin N Am. 1993;1(1):63-78.
- 19. Murakami CS, Larrabee WF. Comparison of osteotomy techniques in the treatment of nasal fractures. Facial Plast Surg. 1992;8(4):209-219.
- 20. Peck GC. Techniques in aesthetic rhinoplasty. New York: Thieme-Stratton. 1984.
- 21. Weir RF. On restoring sunken noses. NYMJ. 1892;56:443.

