This paper reviews the pre, intra and post operatory strategies of a series of abdominoplasties in which the plastic reconstruction of incisional hernia and the practice of an aesthetic dermo lipectomy have been combined. This descriptive retrospective study provides a holistic treatment that resolves not only the pathology but also the abdominal aesthetic. The study is based on a total of 18 patients, who have been treated at the Hospital Domingo Funes (HDF) between the years 2009 and 2019. The involved eventrations proceed from diverse incisions, which brings us to define an amount of specific, universal and common guidelines to all of them. We believe that the execution of this combined procedure is easily reproducible by experienced hands with satisfactory results every time.
Keywords: Abdominoplasties, Dermo lipectomy, Hospital domingo funes
Among the competences of a plastic, aesthetic and reconstructive surgeon, there is the abilities to carry on a repair and reconstruction of functional defects and also defects on the form (both primary and secondary) of the integuments, and of the underlying anatomical systems (including the abdomen), trying to achieve an aesthetic result in the procedure.1
Abdominoplasty is one of the surgical procedures of our specialty, on which countless technical variants have been proposed that adapt to multiple surgical findings. If to the numerous purely aesthetic technical variants, we add those of reconstructive plastic aponeurotic muscle of the abdomen, the arsenal available to the surgeon to face this challenge is enormous.
The Hospital Domingo Funes, located in Villa Caeiro, Córdoba, counts on a significant number of patients who hope to resolve their hernial pathology and, at the same time, to obtain a better appearance of their abdomen. All of these requests led us to rethink what the real competences of our specialty are (plastic, aesthetic and reconstructive surgery) and which attitude we should have towards these cases.
Personally, I believe that our specialty´s main objective is to train the best qualified surgeons who will be able to perform not only an abdominal aesthetic, but also an ad integrum plastic reconstruction of the aponeurotic muscle wall of the abdomen from a dynamic point of view.
Moreover, let's remember the objectives that a reconstruction of the ideal abdominal wall must cover2
- Prevent a visceral eventration Provide adequate coverage Achieve tissue stress-free repair
- Achieve appropriate dynamic muscle support Achieve an adequate aesthetic result.
With regard to the fourth point, it is necessary to bear in mind that the abdominal muscles are not a mere structural support of viscera, they have several functions3
- Control intra-abdominal pressure changes coordinated with the breathing and the floor of the pelvis.
- Achieve the movements of the trunk.
- Postural balance of the spine and maintaining the center of gravity.
- Collaborate with pressure changes in defecation, urination, cough, etc.
Some studies reviews show that, when the repair of incisional defects of the abdominal wall is combined with aesthetic panniculectomies, the number of postoperative complications, such as seromas, cellulitis, necrosis and dehiscence, rise.4,5 What is worse, all of these complications would then be associated by the patient with the experience of the surgeon and quality of institution.6
On the other hand, there are other publications that consider the resolution of the musculo- aponeurotic pathology of the abdominal wall, together with dermo fat aesthetic correction, to be opportune and beneficial.7,8
This is a retrospective descriptive study that includes functional/aesthetic abdominoplasties performed at the Domingo Funes Hospital (HDF) from 2009 to 2019.The inclusion criteria considered were: the presence of giant or multiple ventral eventrations, or giant ventral hernias. Los de exclusión fueron: el del incumplimiento de cualquiera de las indicaciones de la preparación pre quirúrgicao la negativa a la firma del consentimiento informado. Those excluded were: non-compliance with any of the indications of the pre-surgical preparation or refusal to sign the informed consent.
The variables analyzed were:
- Previous surgery origin of the incisional hernia.
- Type incision of previous surgery.
- Operative and perioperative strategy for the resolution of the case.
- Complications.
Pre surgical preparation
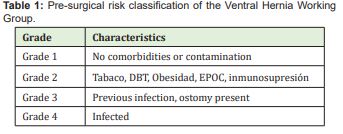
Patients were asked for laboratory studies, including complete cytologic, complete coagulogram, glycemia, ionogram, uremia, creatinine and proteinogram; X-rays of the chest and abdomen standing. At this stage, interdisciplinary work is key. An accurate preoperative evaluation of the patient,9,10 should be performed as proposed by the Ventral Hernia Working Group11 in the following Table 1. In order to be accepted into this procedure, the patient had to decrease its Body Mass Index (BMI) to values that did not exceed 35 kg / m2. Therefore, the Nutrition Service evaluated the eating habits of the patients and planned their diets according to the objective.
The kinesiology and physiotherapy service instructed patients to perform chest breathing exercises, as well as aerobic activities, to help them lose weight and tone their muscles. Plus, the Medical Clinic service evaluated, controlled and/or corrected the cardiac, hypertension, endocrinological or other problems presented by the patients.
Finally, the Pneumonology service performed a spirometry to authorize the procedure and to define the perioperative pharmacological therapy that should be followed. It is vital to add that those patients who are classified as smokers should quit that habit at least 3 months before surgery and resume it at least after 3 postoperative months.
Patients were instructed to use a low-elasticity compression girdle and to place a high- density foam plug lined in cotton cloth in the incisional hernial orifice. The girdle has to be placed by a third in a supine position, with the abdomen relaxed and should be girded progressively over the days. The objective of this measure was to recover the domicile of the intra-abdominal viscera and promote thoracic respiration.
The ambulatory preparation of the skin of the abdomen consisted of: Sanitize it at least once a day with neutral soap. Keep the skin free of moisture, mycoses and injuries such as sloughing, furunculosis, irritations, etc. Perform a moisturizing treatment with water-based cream plus vitamin C throughout the abdomen.
Use a cotton shirt or T-shirt that absorbs moisture. Preoperative thromboembolic prophylaxis was performed with low weight heparin at a dose of 0.75 mg/kg and cephalotin antibiotic prophylaxis 1,000 mg (in case of allergy to penicillin, ciprofloxacin 400 mg) 30 minutes before starting the procedure.
Although it is true that the Surgical Antibiotic Prophylaxis Guide of the Argentine Society of Infectology recommends NOT prolonging the use of antibiotics in clean and clean-contaminated surgeries, even with drains, implants or polypropylene meshes9, in our experience and, according to the social conditions of our patients, we believe that it is better to maintain antibiotic support for 72 hours postoperatively.
Surgical Strategy
The combined aesthetic and functional approach of the abdomen with eventogenic pathology allows the patient to resolve both conditions in a unique surgical intervention, with all the economic, medical and time investment benefits that implies. Firstly, it is necessary to have an idea, as close as possible to reality of the characteristics of the patient's abdominal wall. In order to know this, we requested a Computed Axial Tomography (CT) with an oral and intravenous contrast, a resource that we count on at our hospital.
In the cases of median, para-median, oblique and transverse supra-umbilical eventrations, an anchor or Liz flower design was made for the execution of dermo lipectomy Figure 1.

Regarding the infra-umbilical eventrations, it will depend on the particular characteristics of each case. For better exemplification we opted for a conventional dermo lipectomy, known as a TULUA, or an anchor or Liz flower.
From the surgical approach, the incision was made with a margin of conservative dermo fatty tissue, once the plastic of the aponeurotic muscle wall is completed, the resection is adjusted according to the patients demand.
The repair of the incisional hernia was resolved by the surgeon closing the cut without tension or with low tension performing, if necessary, discharges in neighboring structures.
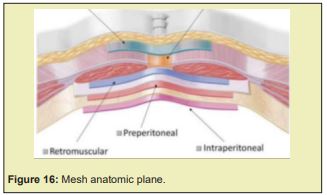
In all patients, polypropylene mesh was placed in the preperitoneal or interaponeurotic space12. The technique is extraperitoneal, if the patient does not have mechanical intestinal involvement due to adhesions or multiple corners of the sac, the abdominal cavity is not entered.
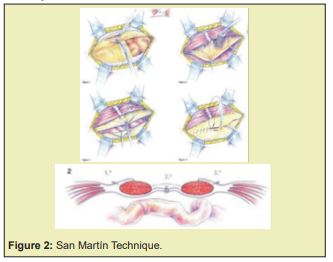
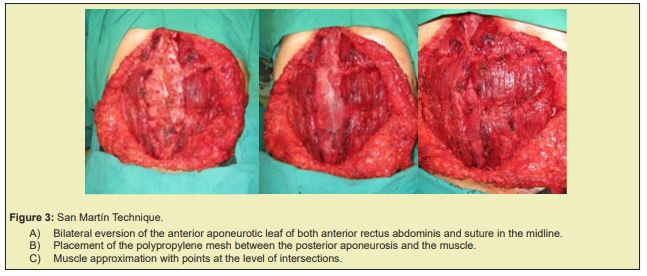
Specifically in median eventrations, if primary closure was possible, the mesh was placed in the preperitoneal space. In those cases in which the width of the defect did not allow its edges to be approached without tension, the San Martín technique was chosen, which consists of the placement of the mesh in the space between the posterior aponeurosis of the anterior rectus and the muscle itself.12
The technique of A. F. San Martín (Argentina, 1943, 1948), unifies the proposals of Gersuny (decapsulation of both anterior recti of their anterior and posterior aponeurotic sheaths, and suture of the first in the midline), and that of Noble (bilateral carving in shutter of the anterior leaf of both rectal sheaths, overturned and sutured on the defect). His technique is described as the section of the anterior sheaths of both recti, which are carved and turned over the hole, covering their herniated area and sliding both rectus muscles medially Figures2,3. Once the incisional hernia was resolved, the definitive dermo lipectomy was measured and adjusted, then performing isolated points of vicryl nº 1 from the dermo fatty flap to the aponeurosis, both to reduce the tension in the middle suture line, as well as the possibilities of seroma formation. Then the closure of the subcutaneous cell tissue was performed with a continuous suture with Vicryl nº2 in two planes, intradermal with colorless Vicryl 3-0 and adjustments with nylon 5- 0. Bandage with Micropore tape and closed aspiration drain.
Immediate and mediate postoperative
Early ambulation (the same day of surgery) was encouraged and hospital discharge was done 24 hours after surgery. The closed aspiration drain was removed when the debit is less than 60ml/24 hours. A gentle pressure band was placed for 72 hours, which had to be adjusted progressively the following days. Due to the characteristics of our environment, the posterior follow-up of the postoperative period was extremely difficult. The main cause is related to the financial and economic status of the patiences that assist at this institution, as the vast majority work in rural areas far from urban centers (more than 100 kilometers from the hospital). Plus, they have severe communication difficulties (lack of telephone signal) and do not count on many ways of transport.
During this period, 18 of the patients that were intervened, 10 (55.5%) were women and 8 (44.5%) were men, both ranging between the ages of 42 to 67 years. The primary surgeries that resulted in eventrations were: 3 (16.6%) cholecystectomies, 3 (16.6%) appendectomies, 2 (11.1%) gynecological, 6 (33.3%) trauma and 4 (22.2%) other acute inflammatory abdomens.
Of the total procedures, 3 (16.6%) had Kocher incision eventrations, 1 (5.5%) Rockey incision, 3 (16.6%) median infraumbilical, 1 (5.5%) right infraumbilical pararectal, 2 (11.1%) median supraumbilical, and 8 (44.4%) median supra-infraabdominal.
The total number of patients (100%) underwent surgery with spinal anesthesia combined with infiltration with modified Klein solution and deep sedation or neuroleptoanalgesia. Surgical time ranged from 200 to 270 minutes.
Polypropylene mesh was placed in the preperitoneal space in 13 (72.2%) of the cases, interaponeurotic in 1 (5.5%) opportunity and, in 4 (22.2%) cases in the space located between the posterior aspect of the anterior rectus abdominis and its posterior aponeurosis.
The complications that occurred were all minor and were solved by ambulatory means: 2 (11.1%) infections of a small segment of the dermal suture, and 4 (22.2%) necrosis with dehiscence, 1 (5.5%) neo umbilical, and 3 (16.6%) of the crossing of the incisions in the anchor or fleur-de-lis design.
There are several classifications of incisional hernias,13 all very similar and with their deficiencies, which respond to the great diversity of presentations observed in this pathology. The most commonly used classification is the one of the European Hernia Society (EHS).14
This classification of postsurgical eventrations is based on location and size criteria. Based on those criteria, they are divided into midline eventrations (M), which is subdivided into 5 areas ranging from the xiphoid apex to the pubis; and on sides (L), which is subdivided into 4 areas as shown in figure 4. In addition, depending on the maximum transverse diameter they are cataloged (table 1) as W1 (<4cm), W2 (≥4–10cm) or W3 (>10cm) Figure 4.

If we intend to carry out this combined procedure, which brings significant benefits to the patient, such as economical ones, having to allocate time and effort to a single postoperative period, and fewer anesthesia, hospitalizations and admissions to the operating room; the meticulous study of the patient is essential.
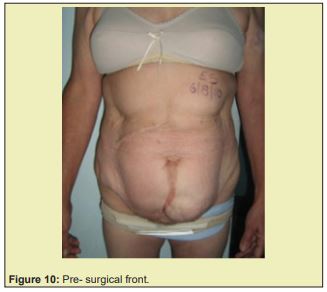
The correct pre-surgical evaluation of both clinical and psychological patients and their meticulous preparation is key. Extreme care must be taken and possible complications must be anticipated, the intervention should not be carried out until the conditions are optimal, containing the patient, without yielding to their demands for prompt resolution even at the cost of this deciding to leave us and look for another professional, as has happened to us on several occasions and that perhaps could be avoided with regular support from the mental health team Figures 5.

When in presence of a difficult-to-solve abdome, the anchor tummy tuck ends up being the best solution for this cases15,16 Figures 6-12.

The dermo fatty incision line must be kept not only for a greater margin of safety for closure in case any unexpected complication appears during the procedure, but also to be able to later execute a musculoaponeurotic plastic surgery, so as to adjust resection of the flap with greater precision. Besides, by doing the final diaeresis at the time of closing, we make sure that all edges of the future suture are just sectioned and have less contact time with air, which will consequently reduce the chances of future consequences with the suture.
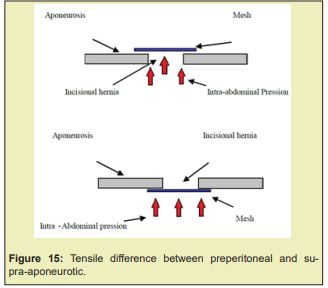
Like the wall of a dam lays on the mountain to be able to deal with the pression of the body of water Figure 13, the collocation of the polypropylene mesh in the preperitoneal space is substantial to better the functional results and the tensile strength Figure 14. On the other hand, as it is separated by the aponeurosis of the fatty detachment space, its responsibility to produce seromas is eliminated, just like its contamination and exposure due to issues with the closure of the wound.17
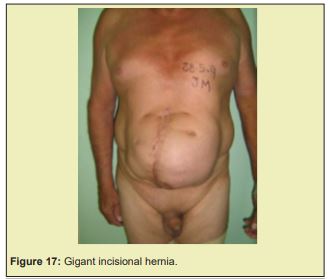
In case of giant eventrations of the midline, the liberation of the major obliques does not ensure coaptation of the lips of the incisional hernia, and this technique requires a large detachment of the dermo fatty flap and aponeurotic muscle. Therefore, we prefer the San Martín Technique with colocation of the mesh in the preperitoneal space. If the situation does not allow its position there, then it is possible to do it in between the posterior aponeurosis of the rectus femoris and the muscle itself, which, one it is released of its adhesions, it broadens and covers all the mesh Figure 15-17. These two options had proven to have a lower infection rate than placement in front of the anterior aponeurosis.18





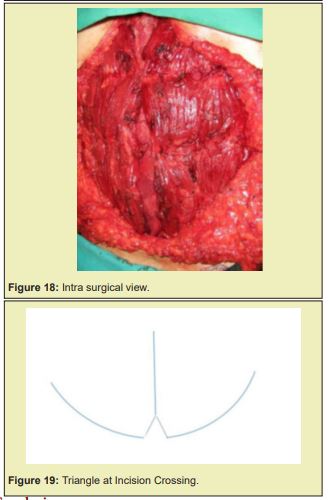
The collocation of stitches from the flap to the aponeurosis, reduces the tension in n the midline suture, improving the final quality of the scar. The necrosis of the crossing between the vertical scar and the Pfannenstiel type that we had at the beginning, we avoided by leaving a small triangular dermal flap on the lower lip of the same, which avoids the 90 degree angle of the flaps Figure 18. The complications we experienced were not as significant as the may seem in the study done by John P. Fischer.5
It is vital that the plastic surgeon has plenty of knowledge of the anatomy of the abdominal wall and dominates various techniques of reconstruction of it so as to be able to choose and modify the surgical plan, if necessary. Our formation as plastic surgeons allows us to have a better control over the soft tissue than other specialties do. Hence, I consider that we are the physicians indicated for the realization of plastic and anatomo-functional reconstructions of the abdominal wall.
It is key to do a correct evaluation and preparation of a personalized preoperative of every patient. The polypropylene mesh should preferably be located in the pre-peritoneal space. If this is not technically possible, in the interfacial area or in the space located between the fascia and the posterior face of the muscle. The resection of the dermo fatty flap must be adjusted on demand once the reconstruction of the abdominal wall has been completed. I recommend the use of the small break in the horizontal scar where it meets the vertical to reduce the chances of ischemic suffering and necrosis.
In our experience, when we perform the combined procedure, surgical time does not last more than 45 minutes. On the other hand, we have not had any major complications that justify splitting the procedures of musculoaponeurotic repair and dermofatty resection. Finally, we believe that performing this compound surgery was correct, coinciding with the results presented by Michael Sosin.19
None.
None.
Authors declare that there is no conflict of interest.
- 1. Especialización en Cirugía Plástica y Reparadora, Res. 524/2.013. SGCS, FCM, UNC, pp. 147.
- 2. Moreno Egea A, Carbonell Tatay F, Vidal Sans J. Técnicas de reparación anatómica: autoplastias. In: Fernando Carbonell Tata, F, Moreno Egea A, editors. Eventraciones. Otras hernias de pared y cavidad abdominal Madrid: Editorial Gràfiques Vimar. 2021;pp.427–442.
- 3. Guías Clínicas de la Asociación Española de Cirujanos, 2ª Edición. Cirugía de la Pared abdominal, Sección de Pared abdominal y Suturas. 2013;pp:42–44.
- 4. Zemlyak AY, Colavita PD, El Djouzi S, et al. Comparative study of wound complications: isolated panniculectomy versus panniculectomy combined with ventral hernia repair. Journal of surgical research. 2012;177(2):387–391.
- 5. Fischer JP, Tuggle CT, Wes AM, et al. Concurrent panniculectomy with open ventral hernia repair has added risk versus ventral hernia repair: an analysis of the ACS-NSQIP database. J Plast Reconstr Aesthet Surg. 2014;67(5):693–701.
- 6. Koolen PGL, Ibrahim AMS, Kim K, et al. Patient selection optimization following combined abdominal procedures: analysis of 4925 patients undergoing panniculectomy/abdominoplasty with or without concurrent hernia repair. Plast Reconstr Surg. 2014;134(4):539e–550e.
- 7. Shermak MA. Hernia repair and abdominoplasty in gastric bypass patients. Plast Reconstr Surg. 2006;117(4):1145–1150.
- 8. Cheesborough JE, Dumanian GA. Simultaneous prosthetic mesh abdominal wall reconstruction with abdominoplasty for ventral hernia and severe rectus diastasis repairs. Plast Reconstr Surg. 2015;135(1):268–276.
- 9. Clara L, Angeleri P, Blugerman G, et al. Guía de profilaxis antibiótica quirúrgica. Argentina: Sociedad Argentina de Infectología, 2017;31–32.
- 10. Bernardi K, Adrales GL, Hope WW, et al. Ventral Hernia Outcomes Collaborative Writing Group. Abdominal Wall Reconstruction Risk Stratification Tools: A Systematic Review of the Literature. Plast Reconstr Surg. 2018;142(3):9S–20S.
- 11. Khansa I, Janis JE. The 4 Principles of Complex Abdominal Wall Reconstruction. Plast Reconstr Surg Glob Open. 2019;7(12):e2549.
- 12. Sosin M, Nahabedian MY, Bhanot P. The Perfect Plane: A Systematic Review of Mesh Location and Outcomes, Update 2018. Plast Reconstr Surg. 2018;142(3 Suppl):107S–116S.
- 13. Muysoms FE, Miserez M, Berrevoet F, et al. Classification of primary and incisional abdominal wall hernias. Hernia. 2009;13(4):407–414.
- 14. León Ledesma R, Guillén Morales C, Limones Esteban M. Hernia ventral: concepto, epidemiología y clasificación. Guías Clínicas de la Asociación Española de Cirujanos. Cirugía De La Pared Abdominal 2ª Edición. 2013;pp:137–140.
- 15. Soria JH, Tuero A, Noé G, et al. Nuestra conducta en la asociación de hernia de pared y abdominoplastia estética. Cirugía Plástica IberoLatinoamericana. 2016;42(2):157–166.
- 16. Roxo CPD, Roxo ACW, Almenares MC. Abdominoplastia multifuncional: estudio retrospectivo de 5 años de experiencia con 108 pacientes. Cirugía Plástica Ibero-Latinoamericana. 2008;34(3):201–210.
- 17. Albino FP, Patel KM, Nahabedian MY, et al. Does mesh location matter in abdominal wall reconstruction? A systematic review of the literature and a summary of recommendations. Plast Reconstr Surg. 2013;132(5):1295–1304.
- 18. de Vries Reilingh TS, van Geldere D, Langenhorst B, det al.. Repair of large midline incisional hernias with polypropylene mesh: comparison of three operative techniques. Hernia. 2004;8(1):56–59.
- 19. Sosin M, Termanini KM, Black CK, et al. Simultaneous Ventral Hernia Repair and Panniculectomy: A Systematic Review and Meta-Analysis of Outcomes. Plast Reconstr Surg. 2020;145(4):1059–1067.

