- Primary intraosseous cavernous hemangiomas (PICHs) is a rare hemangioma in the skull. The diagnosis and treatment need to be coordinated by related specialties, in which the gold standard for diagnosis is histopathology.
- The clinical case is a 72-year-old male patient with a parietal frontal hemangioma originating in the skull, which is an intracranial cavernous hemangioma.
- Treatment was consisted of vascular intervention, total cranioplasty, covering with an artificial material and a skin flap.
- The patient underwent 3 surgeries to remove the tumor, the second time the pathological result was a cavernous hemangioma of the skull.
Keywords: Cavernous hemangioma, Intraosseous skull cavernous hemangiomas, Primary intraosseous cavernous hemangiomas, PICHS
Hemangiomas are benign soft tissue tumors, usually in the skin of newborns and children. Hemangiomas may appear in other tissue including muscle, tendon, connective tissue, fatty tissue, synovial fluid, or bone.1 Hemangiomas are histologically classified on the basis of vascular channels including capillary hemangiomas, cavernous hemangiomas, venous or arteriovenous hemangiomas.2-6 In particular, primary intraosseous cavernous hemangiomas can occur anywhere in the body. PICHs is an extremely rare disease, accounting for only 0.7-1% of bone tumors, and 10% of benign skull tumors. PICHS are common in middle age (40-50 years old), male/female ratio is about 3/1 to 2/1.67. PICHS has an unclear pathogenesis, which may be related to a history of trauma.2,5,6,7
It was first described in 1845 as a case of cavernous hemangioma originating from the parietal bone, by 2016 only 93 cases had been reported. PICHs originates from the space between the two plates of the skull and is supplied with blood by the external carotid artery.1,2
Common clinical symptoms include enlarged skull, with or without pain, headache, dizziness. Localized neurologic findings are uncommon because the tumor tends to grow outward. Eyelid ptosis and visual impairment may occur if the tumor compresses the orbit, paralysis of VII or hearing loss when in the temporal bone.2,5
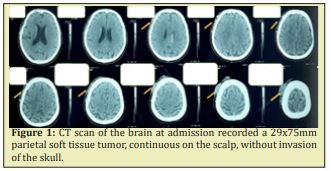
A 72-year-old male patient with no history of hemangioma, headache, dizziness, head trauma, radiation therapy or chemical exposure. The patient was found to have a vascular tumor in the scalp that was gradually getting bigger, and was removed at a hospital, the surgical wound then kept bleeding and did not heal. At the time of examination, his general condition was stable, the hemangioma in the top forehead was hard and not mobile. On the computed tomography (CT) image, a soft tissue tumor of the apex 29x75mm, continuous on the scalp, has not yet invaded the skull Figure 1. Histopathological results: microvascular hemangioma, chronic ulcerative colitis.
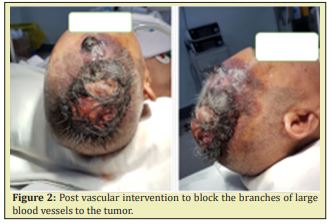
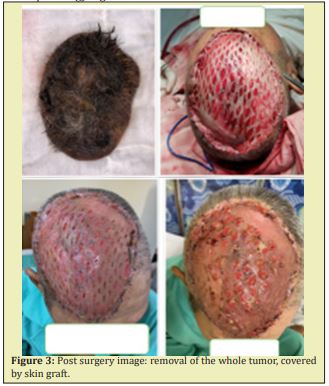
First vascular intervention: occlusion of the great branches to the tumor from the bilateral external carotid arteries (superficial temporal arteries) and the right internal carotid artery (middle meningeal artery) Figure 2, surgical resection of the entire hemangioma to galea layer, skin defect was then covered by skin graft Figure 3.
Two weeks post-surgery, recurrent tumors were found, they rapidly increased in size with necrosis and bleeding tissue Figure 4.

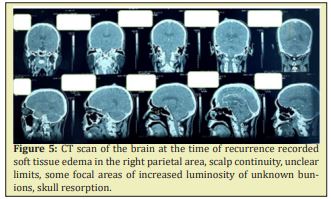
CT scan of the brain recorded soft tissue edema in the right parietal area, scalp continuity, unclear limits, some focal areas of increased luminosity of unknown bunions, skull resorption Figure 5. Second vascular intervention: blockage of a few small capillary-shaped branches to the tumor area from external carotid artery. A surgery was performed to remove necrotic tumor tissue after vascular intervention, and to remove the extracranial plate for exploration. The observation showed many points of vascular communication from the base of the skull to the skin, we took a sample for histopathology Figure 6.

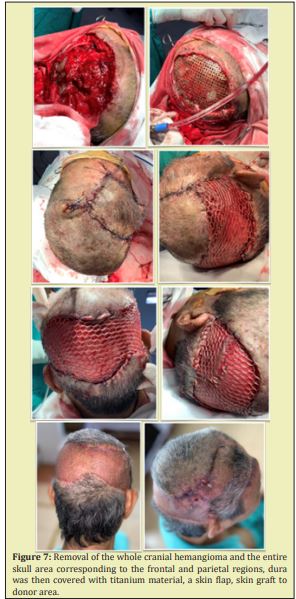
Histopathological results showed cavernous hemangioma in the skull. The patient underwent surgery to remove the whole cranial hemangioma and the entire skull area corresponding to the frontal and parietal regions, dura was then covered with titanium material by a neurosurgeon, the artificial material was then covered with a skin flap, skin graft to donor area by plastic surgery specialist Figure 7. The patient was followed up 4 weeks later, the skin graft healed well, the artificial material was completely covered, no focal neurological signs were noted.
Primary intraosseous cavernous hemangiomas is a very rare disease that can occur anywhere in the body. PICHs is more common in the spine than in the skull, in the group of tumors occurring in the skull, it is more common in the parietal and temporal bones.2,5,6,7 The diagnosis is based on clinical, radiological, and most importantly, histopathology. The imaging tools that can examine cavernous hemangiomas include X-ray, CT scan, and MRI. In particular, CT scan is an excellent means of surveying, clearly showing widespread lesions in the skull, images of internal and external cranial erosion when the tumor proliferates. However, PICHs in skull bones do not have typical imaging features, which must always be distinguished from other lesions: metastatic tumor, sarcoma, fibrous dysplasia, Paget... Therefore, histopathology is the diagnostic criterion, imaging helps determine the location, size and extent of the lesion.2,6,7 For intraosseous cavernous hemangiomas, treatment is indicated when the tumor is large, causing bleeding or in need of cosmetic improvement. Total resection is the optimal treatment with a safety margin of 0.5cm3,4 then covered with titanium. Tumor angiography and preoperative vascular intervention are recommended by many authors, especially with large tumors, in order to reduce tumor size and reduce intraoperative blood loss. Common large vessels include the middle meningeal artery, superficial temporal artery, and posterior occipital artery. In our clinical case, we also recorded and intervened these blood vessels before surgery, the preoperative intervention minimized blood loss and helped clear the surgical field when resecting the tumor. Radiation therapy alone helps to stop the tumor from multiplying, it does not remove the tumor. The rate of recurrence is very rare if it is completely resected.2,6,7
Primary iintraosseous cavernous hemangiomas of the skull is a very rare disease, presenting similar to some other tumors in the soft tissue of the head. The diagnostic gold standard is histopathology and imaging that aid in the diagnosis in determining the location, size, and extent of spread. Treatment requires the coordination of many specialties including pathology, imaging, vascular intervention, neurosurgery, vascular surgery, and plastic surgery.
None.
None.
All authors declare no conflict of interest.
- 1. Sáenz AA, Porto NF. Sánchez MP. Intraosseous cavernous hemangioma: presentation of a clinical case. Egypt J Neurosurg. 2018;33:22.
- 2. Yang Y, Guan J, Ma W, et al. Primary Intraosseous Cavernous Hemangioma in the Skull. Medicine (Baltimore). 2016;95(11):e3069.
- 3. Lok Huei Yap Howard N. Langstein. Reconstruction of the Scalp, Calvarium, and Forehead in Grabb and Smith’s Plastic Surgery 6th. 2007; p. 358–366.
- 4. Karen H Kim, Roy G Geronemus. Mohs micrographic surgery in Grabb and Smith’s Plastic Surgery 6th. 2007; p. 116–119 .
- 5. Aurora A, Krishnan MM, Bahadur R, et al. Cavernous hemangioma of the frontal bone: A case report. Indian J Ophthalmol.1991;39:76–77 .
- 6. Bravo Martinez A, Marrero Gonzalez AP, Suleiman Suleiman MN, et al. Radiologic Features with Pathologic Correlation of an Unusual Large Intraosseous Skull Cavernous Hemangioma. Am J Case Rep. 2019;20:525–530.
- 7. Liu JK, Burger PC, Harnsberger HR, et al. Primary Intraosseous Skull Base Cavernous Hemangioma: Case Report. SkullBase. 2003;13(4):219–228.

