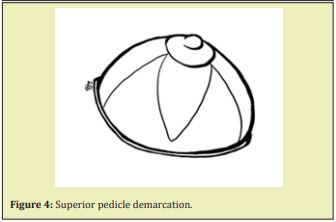
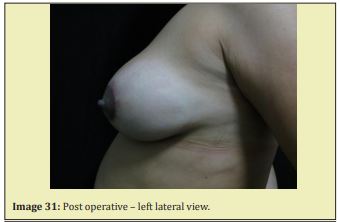
The author approaches circumareolarar aesthetic mammoplasty using this technique. Internal treatment of the breasts may be carried out by keel resection of the side pillars and Mastopexy (previously published work), or by the technique presented here - forming a superior pedicle flap of fatty and glandular tissue, 5cm wide and of variable length, introducing it into the upper pole for added projection and volume and bringing together the lateral pedicles mastopexy by continuous suture to the muscle fascia, continuing the suture up to near the entrance at the base of the flap in the areola and ending about 2.5 centimeters from its base. Shaping can be carried out in the new breasts, if required, either superiorly or inferiorly, in order to improve their shape(tapering). Liposuction can also be performed to achieve better cosmetic results.
Keywords: Circumareolar mammoplasty
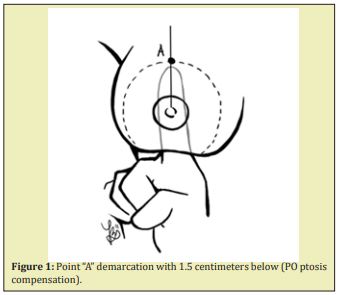
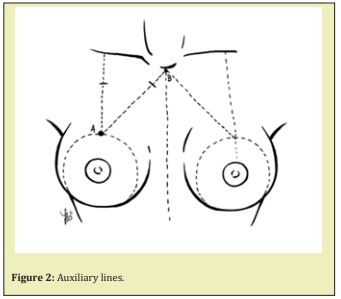
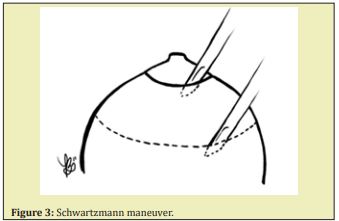
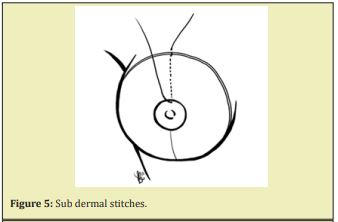
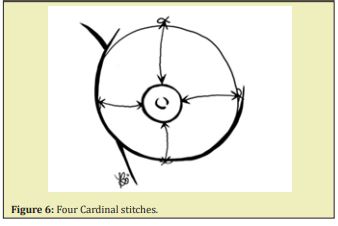
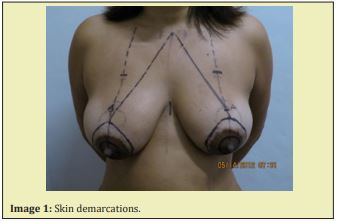
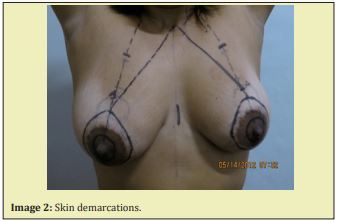
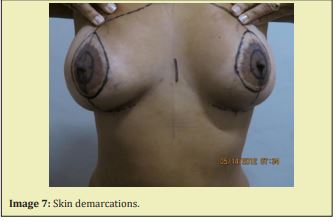
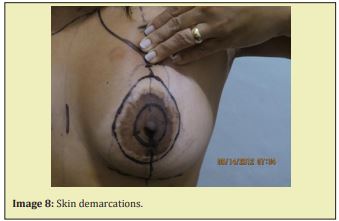
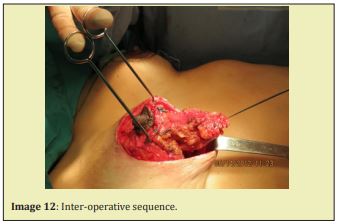
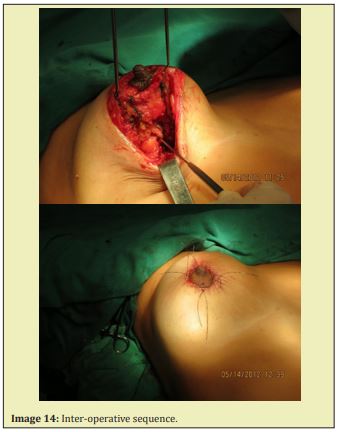
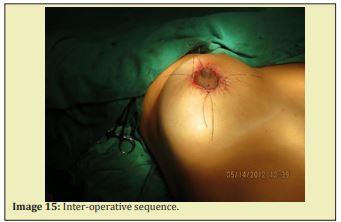
Draw a line midclavicle to the inframammary fold. On this line, we place the point A (Figure 1) 1.5 centimeters below its original position; this ensures that the final position of NAC is correct (post op breast ptosis compensation). We then determine the area to be resected (Figure 3) (circumareolar) and the final size of the chosen areola. The area to be resected can then be removed using the Schwartzmann maneuver. An auxiliary line of demarcation comes from the sternal notch to point A (Figure 2) the ideal length ranges from 21 to 22 centimeters. We select a point on the midclavicular line ten centimeters down from the clavicle, that serves as a reference point. The Schwartzmann maneuver should be carried out as superficially as possible in the sub dermal and cellular subcutaneous tissue, as this better preserves nipple/areola sensitivity. Extensive work in this subject has already been conducted and scientifically proven. Our choice of superior pedicle is because of the proven superiority of the vascularity of the breasts in their upper middle region (angiograms) (Figure 5). If the distance between the two circumareolar demarcations is over 2.5 centimeters, we change to an elliptical demarcation in the upper portion; otherwise we could sacrifice final results. After resection of the internal glandular and adipose tissue it is unnecessary to exposure the pectoral aponeurosis (EH Findley). The pexia of the inferior part of remaining pillars on the pectoral aponeurosis is questionable. Despite its questionable efficacy in the long term, we still perform this routinely by means of a continuous suture of monofilament nylon 3.0 working top-down to the areola (Figure 6) and then returning to the top position. The pillars are brought together with 3.0 simple running sutures. The total ineffectiveness of adipose tissue sutures and the limited effectiveness of glandular tissue sutures should be born in mind. We then proceed to the reshaping of the breasts. If we choose so, this can be done superiorly, in the upper pole, or inferiorly. The skin will cover the breasts formed by us but will not shape them. With regard to the circumareolar suture, the greatest challenge of this surgery, puckering, can be alleviated as follows: carry out a large detachment outside the outer demarcation; otherwise the areola will enlarge. We are aiming to retain the original size. First we perform four cardinal stitches of 4.0 monocryl (poliglecaprone 25) or 3.0 PDS II (polydioxanone) and then we bring together the deep dermis between these stitches with a running suture of 3.0 nylon monofilament, and finally an intradermic running suture with Monocryl or PDSII (Figures 8,9). The Nylon suture can be removed after two or three weeks. We use no drains after surgery, micropore in small pieces over the areola incision, and thermoplastic adhesive in siliconized paper in the middle lower portion of the breasts and bra for eight weeks, 24 hours a day.1-8
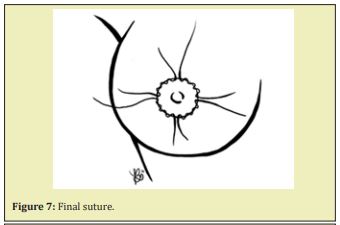
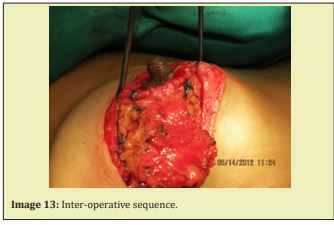
We believe that this technique serves well for cases of small and medium hypertrophy with or without ptosis which require a reshaping of the breasts and a reduction in size and lifting of the NAC to a higher position with little scarring. The final scar tends to improve with time and since we do not use synthetic non-absorbable material (formation of sinus, hypertrophic scar and extrusion of stitches) the final scar will be very acceptable (Images 1-32).























None.
None.
Author declares that there is no conflict of interest.
- 1. Paoliello Victor. Mamaplastia Peri-areolar Personal Approach. Brazilian Journal of Medicine. 1993;65(4):179–182.
- 2. Hall Findlay J. Vertical Breast Reduction with the medially based pedicle. Operative Strategies. Aesthetic Journal. 2002;22(2):185–194.
- 3. Schwartzmann E. Avoidance of nipple necrosis by preservation of corium in one-stage plastic surgery of the breast. Rev Chir Struct. 1937;7:206-209.
- 4. Strombeck JO. Mammaplasty: reports far new technique based on the two-pedicle procedure. Br J Plast Surgery. 1960:13:79–90.
- 5. Lejour M. Vertical Mamaplasty and liposuction of the breasts Louis: Quality Medical Publishing. 1993.
- 6. Felicio Y. Journal of Surgery. 1989;79(3).
- 7. Pitanguy I. Hipertrofias mamárias. Critical study and personal technique. Rev Bras Cir. 1966;51:263.
- 8. RASPS. Recents Advances in Plastic Surgery Annals of the International Symposium. 1989.

