An increasing number of studies across multiple fields demonstrate an association between individuals’ built environments and their health, indicating the value of intentionally designing spaces for well-being. However, the application, accessibility, and advancement of this research remains limited. Given the emerging nature of this field, it is important to gather thought leaders in this work to obtain their insights regarding current efforts and next steps.
This qualitative study used convenience and snowball sampling to convene international experts representing multiple disciplines (n=13) to participate in four focus groups, in which they described the state of the field of health and the built environment; made recommendations for research and practice; and discussed challenges and opportunities. Subsequent thematic analysis of transcripts was iteratively conducted by an interdisciplinary, inter-institutional research team, resulting in six themes: Opportunity, Engagement, Interdisciplinarity, Research, Funding, and Recommendations. Participant priorities included the need for public and professional awareness, interdisciplinary collaboration, funding, improved research, and equitable application.
Discussions illuminated action steps and overarching directions for the field. On the whole, findings indicate that important opportunities exist to improve health and well-being outcomes through design, architecture, and the built environment, and that robust interdisciplinary processes could help ensure these opportunities are taken up to further support health and health equity.
Keywords: Interdisciplinary, Qualitative, Built environment, Architecture, Design, Well being
An increasing number of studies across multiple fields demonstrate an association between individuals’ built environments – man-made structures where humans “live, work, worship, learn, and play” – and their health.1-3 For example, findings indicate that when environments are designed for well-being, they can decrease depression and stress, support school attendance and higher standardized test scores, improve mood and subjective well-being, and increase physical activity.2,4-8 More specifically, there is increasing recognition that stressors such as noise, crowding, housing type, light, and air quality in the built environment can all affect quality of life,9 and that the vitality or liveliness of a place can increase positive affect—promoting a sense of affiliation and protecting from urban loneliness.10 Integrating shared or public neighborhood facilities such as libraries and recreation centers has been shown to improve social connection and encourage exercise, and neighborhood designs such as garden spaces have been found to enhance one’s sense of community and improve quality of life.11-14 In fact, simply looking at photos of desirable or undesirable landscapes has been shown to influence one’s anticipation of threat—a phenomenon linked to increased depression, anxiety, and paranoia.15,16
As understanding grows regarding the health effects of built environments, research has increasingly called for interdisciplinary collaboration to create more psychologically sustainable environments.17,18 8 This can be clearly seen in the emergence of neurourbanism, an interdisciplinary approach linking neuroscience, planning, public health, epidemiology, architecture, and other relevant fields.19 Similarly, neuroarchitecture and the psychophysiological study of urban stressors have developed with a goal of investigating relationships among urban architecture, density, landscapes, and the human brain.18 Meanwhile, schools, hospitals, clinics, and other community settings are increasingly considering how art, green spaces, and design choices such as biophilic strategies can improve health outcomes.7,20-23
Such findings suggest that, far from mere “nice-to-haves,” health-supportive environments may be essential tools, assets, and considerations in health care and public health. However, the many disciplines involved in related work (e.g., design, psychology, urban planning, architecture, education, neuroscience) vary in how they describe, conduct, and report studies.24 In addition, interdisciplinary efforts appear to be hampered by the methodological, conceptual, and structural challenges of integrating knowledge across domains.25
In response to both the promise and current challenges of improving built environments, the International Arts + Mind Lab (IAM Lab) partnered with the Academy of Neuroscience for Architecture (ANFA) in 2021 to develop the "Intentional Spaces" initiative. This project and its title reflect the idea that spaces can be intentionally designed, built, and utilized to support human health and well-being. The word “spaces” indicates the initiative’s focus on built environment and design (within the sweeping scope of environmental health), and the fact that settings under consideration may range from specific rooms to entire buildings to urban design. On the whole, this initiative aims to 1) generate truly interdisciplinary discussions regarding effects of spaces and settings on human health and wellbeing; and 2) optimize current knowledge while cultivating research that addresses gaps in the field. At the core of the initiative is an interinstitutional working group of scientists, architects, and designers whose careers include a focus on the health impacts of the built environment.
This qualitative study is the initiative’s foundational effort. The study convened international experts across fields of architecture, neuroscience, design, urban planning, creative placemaking, and more to identify participants’ impressions of the state of the field, elicit their recommendations for research and practice, and foster interdisciplinary discussions regarding current gaps, challenges, and opportunities. Beginning with a small-scale study that will inform and spur additional research endeavors, the aim of this work is to provide a bedrock for advancing our collective understandings and applications of spaces’ effects on health and well-being.
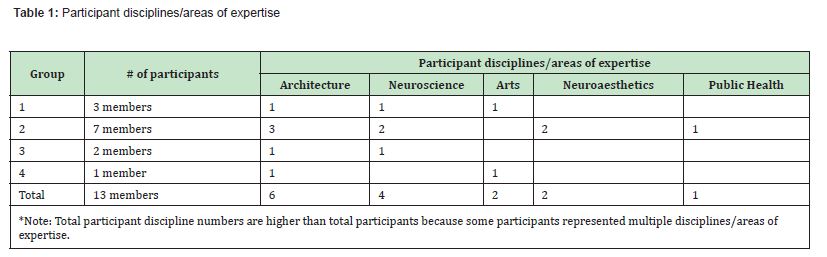
To begin this study, the “Intentional Spaces” working group was asked to recommend experts who are conducting innovative work at intersections of health and the built environment, with the goal of inviting them to participate in focus groups. These experts would then recommend others in their fields, resulting in a snowball sampling process. A total of 75 individuals were ultimately compiled; each was categorized by area(s) of expertise, which included Architecture, Design, Neuroscience, Visual Perception, Technology, Art History, Creative Placemaking, Neurology, Engineering, Museums, and multiple health fields. Next, to support an exchange of ideas across varied backgrounds and areas of expertise, focus groups were curated to represent multiple disciplines. Experts were then emailed an invitation to participate in virtual conversations about “intentional spaces'' and ways to optimize design for positive health impacts. Those who were available to participate selected dates that worked with their schedules; this resulted in three focus groups ranging from two to six participants, and one guided interview (total n=13).
Prior to each meeting, participants were sent biographies of fellow participants to review in advance. Each discussion was led by a member of the IAM Lab, using a facilitation guide to support consistency across groups. Each group heard an introduction that provided a working definition of intentional spaces,[1] described the aim of the initiative to which they were contributing, and defined key terms. The facilitator used the guide to probe experts’ views on the state of the field, strengths and opportunities, challenges, and goals and recommendations. One important question asked during the focus groups was “If you could wave a magic wand and this work would be thriving in the world (in other words, it’s in the best possible place), what would that look like?” Answers to this question provided insight on how participants defined success in the field. The moderator then proceeded to ask further questions about goals for this work, how to measure effects and outcomes, and what needs to be done to achieve success. Groups were also asked what populations and viewpoints need to be brought into the conversation to advance the work and improve equity.
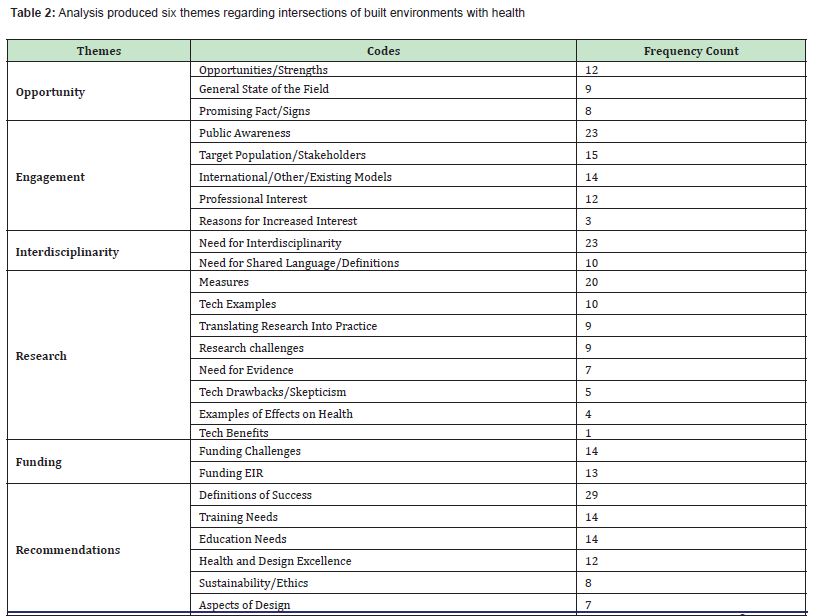
All focus group discussions were recorded, transcribed, and de-identified. Analysis was then undertaken by an interdisciplinary research team consisting of a lead researcher, research coordinator, and four researchers from multiple institutions. Only the lead researcher had been previously involved with the study (as facilitator of three focus groups); to reduce risk of bias, they did not participate in initial codebook development or analysis. Results were analyzed using a theoretical thematic analysis consistent with steps described in Braun and Clarke (2006).26 To begin, a research team member read all four transcripts and created a preliminary codebook. Team members were then paired and assigned two transcripts to code; they also added codes as necessary. Next, each pair met to review and reach consensus regarding coding choices; this resulted in a final codebook consisting of 26 unique codes. The full research team then reconvened to discuss findings across transcripts. Finally, team members created a frequency count for the codes, collectively pulled pertinent quotes to best illustrate each one, and finalized themes.
This study was approved as exempt by the Johns Hopkins Institutional Review Board and all meetings were recorded with permission.
Analysis produced six themes regarding intersections of built environments with health: Opportunity, Engagement, Interdisciplinarity, Research, Funding, and Recommendations. Themes, codes, and frequency counts are documented in Table 2.
Theme I: Opportunity
Regarding the general state of the field, thought leaders observed that significant positive changes have occurred over the last 10-15 years. At the same time, they described a lack of consistent, formalized processes, in both education and practice, for applying architecture and design toward greater health and well-being. They also noted that current efforts to examine health and the built environment tend to focus on the quality of air or water and similar environmental concerns and neglect “the conditions where people can thrive from the sense of mind health.” Current gaps were often framed as opportunities for the field.
Thought leaders also perceived value in knowing why buildings have historically been designed the way they are, and in evolving that process rather than creating something altogether new: “[W]e are not reinventing the wheel, and...there are precedents to do the things that we are trying to accomplish.” In addition, many participants observed a positive opportunity emerging from the COVID-19 pandemic: that more people now recognize the importance of having access to spaces that can support or even optimize health. For example, thought leaders said the pandemic had increased the public’s understanding that the design of buildings and classrooms affects health and educational outcomes, with one person asserting that “design for education is one of the most important priorities in our society today.”
Theme II: Engagement
Broadly defined as the involvement of various stakeholders at intersections of design, architecture, and health, the Engagement theme encompassed the codes “public awareness,” “professional interest,” “reasons for increased interest,” “target populations/stakeholders,” and “international models.”
Public awareness: According to participating experts, a major stakeholder at intersections of design and health is the general public, whose interest was seen as necessary for generating increased demand and therefore more funding. All participants indicated optimism that the public wants spaces to be designed with health and wellness in mind; one respondent even called the public the “third piece of the puzzle” —alongside scholarship and architecture practice—in generating interest and momentum.
However, participants also observed that the public often lacks accessible information about the effects of design and the built environment on health. Some argued that the responsibility for educating the public lies with academics, architects, and other professionals in the field, who “need to make it more known that our environments affect us profoundly.” One participant stated that “our mission should be educating the public;” another said, “If people knew how impacted they were by their physical environment, they would probably want and prefer health-promoting or enriched environments…that make us feel better.” This prompted participants to ask: “How do you…get people to understand that there are other possibilities” beyond what they have come to expect or accept of their environments?
Thought leaders answered this question in three prominent ways. First, many felt that the pandemic-inspired increase in public awareness of buildings’ health effects should be leveraged to move the field forward, though they did not offer concrete suggestions for how to do so. Second, respondents praised models such as the International WELL Building Institute and the Conscious Cities Movement for using scientific knowledge and processes to ascertain users’ needs, and then meet them. For example, the WELL Building Institute certifies buildings as putting users’ health first, provides a seal that certified buildings can display, and then encourages the public to “look for the seal.” Participants argued that this can create public demand for more entities to prioritize health in their building design:
When you introduce metrics that make the human experience visible, you change the whole system. [...] If an environment is known to create positive or negative effects, because of those metrics becoming available, then the owners or commissioners of those environments become responsible and accountable for the decisions of how the design is made.
Finally, respondents stressed the importance of moving beyond the group of experts currently known to be doing this work: “[T]here's too many of the same people in these gatherings,” a participant contended, and intentional inclusivity would advance the field.
Despite an emphasis on public engagement as a path to advancing the intersection of design and health, several respondents expressed concern regarding the low level of influence that individuals typically have over their built environments:
When you think about how much agency you have to change your environment, [it’s] very little. Can you change something on your street? Absolutely not. Sometimes you can't even paint a wall in the house that you've rented. Can you change what kind of businesses...open up in your neighborhood? Can you change the way the city is planned? Can you change the way that transportation is planned? Can you change how things are zoned? No, nothing. And I think that...we are born into this world, and this is the world that we think is normal: that we have zero control over anything, aside from what we might manage to buy with a mortgage.
Professional interest: Interest in this field among students, pre-professionals, and experts in architecture and neuroscience was described as inconsistent, though participants noted that professional organizations like ANFA represent growing investment in collaborative work. Participants also indicated that younger people are increasingly attentive to the effects of built environments on health; one stated that “in the last five or 10 years,” interest among students and younger professionals “has been skyrocketing.”
However, focus groups also mentioned ongoing gaps between academic research and on-the-ground practice (see “Interdisciplinary Challenges”). For example, they mentioned the need to better engage scientists: “We've made some progress in educating the architects about the importance of evidence-based design, but we're not really effective at getting the neuroscience community completely engaged in this problem. There are a lot of great neuroscientists out there, but they're just not…focused on this.” Notably, the assumption that architects have been responsive to the science was complicated by other participants, who expressed the need for “visionary” or “elite” architects to become involved. They also suggested that interest among esteemed architects could be increased by educating them on the health impacts of the built environment, and by clearly indicating how the intersection of design and health could advance their careers.
Reasons for increased interest: Despite recognizing that professional interest must be cultivated, participants indicated they had witnessed growing interest in design for health and well-being in recent years, and speculated about why. Echoing conversations about the pandemic’s influence, several respondents suggested that multiple global events had made people more aware of how the built environment affects their health. One commented that “the whole idea of wellness” has been affected by “the fragility that we've experienced;” as a result, considerations of “how the environment makes you feel, and…creating the conditions where you can thrive and do your best thinking and your best work, seems to be radiating with people.” Another participant highlighted the impact of the Black Lives Matter movement on the built environment, saying that “everybody is beginning to...look at ecology as a bigger circle…that talks about civic health and societal health, and economics.” This individual expected that collaborative work at intersections of design and health will grow as “the younger generation [is] politicized.”
Participants also traced growing interest in design and health to the fact that community residents and decision makers increasingly value factors other than cost. One asserted that the “real costs” are the “people within [the buildings], and whatever they’re doing,” and noted that current leaders are “very interested in that.” Another elaborated on this, arguing that the “real costs” of building extend to wellbeing and health; as a result, optimizing efficiency and return on investment requires that health impacts be better integrated into design. As one person stated, “When you discuss with [CEOs and community leaders], the question is, why is it important? You know, why are we doing this? And the thing that I think they seem to get is [that] it does relate to…flourishing and the human condition, that by creating these environments…it strengthens their community.”
Target populations/stakeholders: In addition to discussing public awareness and professional interest, focus groups were asked who was missing from current conversations about effects of design and the built environment on health. Responses were wide-ranging, including psychologists to inform “trauma-informed practices” and how to “do no harm” in building design, as well as economists, who could potentially “do a full economic life cycle analysis of the building.” A practicing architect said they “deal with more of the CEOs or the leaders of organizations,” and that these groups should be included in conversations about the health effects of design. Another participant added that major foundations are often missing from these conversations, and the resulting lack of funder awareness ultimately limits funding for related projects. One individual noted the value of well-known figures like Bill Gates, who could easily change the conversation with their influence if they were inclined to do so.
Notably, respondents continually circled back to the importance of including affected communities in decisions about buildings and other spaces. One described a building project in their region that local governmental leaders insisted would be good for the economy. Yet the residents of the affected community repeatedly stated they did not want or need the project, and ultimately, their wishes were ignored. Other focus group members echoed this dissatisfaction with top-down approaches to design—in which a funder brings projects to a community rather than starting with the community first. They also placed emphasis on equity and power imbalances: “I think there's a question of who needs [health-supporting designs] most, right? And who needs it most are the disadvantaged because health is obviously something that the advantaged have very good access to... And so I think really, at the heart of the question is like, where is it most equitable to apply this?”
International models: Many study participants work internationally, providing broad perspectives of ways in which health and wellness are discussed (or not) in, for example, architecture curricula. Some commented that academic research and curricula in the U.S. typically lack international perspectives, resulting in limited awareness of initiatives and processes that are being taught, implemented, and researched around the world. One participant contended that “when it comes to research, and especially architecture and design, there is this great amount of work in East Asia, in Japan, in Scandinavia, that my students, and …we, as architects, we rarely hear about in the U.S.”
Outside research and academia, thought leaders noted that countries appear to differ in how communities are involved in projects related to the built environment. One recounted, “In my research on Japanese architecture, I visited some villages, and I noticed that there were communities in little villages that were extremely engaged in the selection of [building] projects.” Another observed that,
There are a lot more good examples in countries where property law and governance models haven't set…society in a certain way over centuries. And so…in South America and in Africa, I've seen much more interesting examples of how this kind of work can be done, than in places like Europe, or the U.S. where we're so, you know, set in our ways of how the built environment has changed. And I think we have a lot more to learn…I'll put it this way. We have a lot more to unlearn.
Lastly, one participant noted that the success of building projects that prioritize health and well-being often depends on one passionate person who drives them forward. As an example, they mentioned the Urban Thinkscape in Philadelphia— a program that provides opportunities for playful learning in public spaces, and shared that, “The thing that made the project a success was the drive of the community leader to get that project made and have the community involved. That specific person who had that drive was a very strong-willed person. Not every [project] has that.”
Theme III: Interdisciplinarity
Despite witnessing growing interest and willingness to engage in cross-sector collaboration, study participants agreed that there remains a general lack of interdisciplinarity in research and practice, which limits advancement in an inherently interdisciplinary and cross-sectoral field such as health and architecture/design. Participants observed several barriers contributing to this limitation; most generally, they described scientists and architects as “still living in [their] silos.” “Part of the problem,” one person stated, “is that the practitioners are not trained in science, and the scientists are not fully aware of the...practical problems that are facing architects. And so, the only way to make this happen is to bring people together and collaborate.” More particularly, respondents pointed to the lack of shared language, definitions, and priorities among converging fields, which prevents collaborators from designing and implementing projects effectively. One participant said that when they brought researchers and practitioners together to “contrast and compare” efforts, they noticed that the two groups “were both…trying to [reach] the same goals but with methods that were very, very different.”
Responding to these challenges, participants suggested that scientists need to be more inquisitive about architects’ and communities’ lived needs and problems. Additionally, architects and other built environment practitioners need to learn how health research may affect their decisions and processes: “The people who know about science think that design is fluff. And the people who…know about design think that science is irrelevant.”
The challenges of interdisciplinarity led participants to express the value of bringing scientists and practitioners together through trainings, conferences, and opportunities for collaboration. Some went further, emphasizing that such gatherings need to provide a clear structure to guide attendees in effectively connecting and integrating their work:
I always used to compare it to a high school dance with the boys on one side and the girls on the other side and nobody really knowing what to do next… The architects gave the kinds of presentations that architects usually give… and then scientists gave the usual boring empirical talks that we often give. And there was no...mixing it up; there was no genuine discussion of, “how can we inform one another's approaches?”
In short, participants asserted the necessity of developing events or initiatives that bring disciplines and sectors together, but cautioned that intention and effort are required to develop shared practices that lead to genuinely interdisciplinary projects that can be sustained and expanded over time.
Theme IV: Research
Within the Research theme, the following five codes were prominent across all groups: need for evidence, research challenges (i.e., reasons why evidence is lacking), measures, technology, and translating research into practice.
Need for evidence: Participants discussed a lack of research regarding intersections of health and the built environment, tracing this in part to the newness of the field. To build evidence, participants emphasized a need to conduct experiments and increase the amount of relevant literature. Some pointed out that much of the current evidence base comes from “speculations and anecdotal observations,” and that researchers and practitioners in fields such as architecture and design do not yet know “how humans actually behave” and “how they [actually] feel” in various spaces. Ultimately, they argued, “there just needs to be more peer reviewed primary research publications.” One participant hoped that in the future, “every major building project would be a research project,” and others indicated the value of continuing to measure a building’s impact throughout its life.
Research challenges: Discussions about the need for evidence were often followed by mentions of the challenges research presents, and queries regarding how it could or should be undertaken. Participants asserted that although they can measure factors such as heart rate, time spent in rooms/buildings, and satisfaction (see “Measures”), it is nearly impossible to conduct the kind of well-controlled experiments often expected in health sciences. They traced this in part to the sheer number of variables at play when it comes to the effects of the built environment on health or well-being, noting that it is impossible to identify which aspects of the design are actually creating effects unless each variable is accounted for. They further indicated that the validity of measures is an issue when attempting to quantify an experience.
Participants also saw a research barrier in the fact that architects cannot design a building purely for the purposes of experimenting with optimal delivery of positive health effects, because buildings are typically designed in response to clients’ stated needs. In addition, “it’s hard to do experiments in architecture, because it's expensive. You can't change it after you've done it, or at least not very easily” due to costs and other factors. Respondents also opined that architects may be hesitant to conduct experiments or try new things in their designs because it is “not only expensive to make mistakes, but there's also liability issues, you know, they have to sign off on the building, and they could lose their certification.”
Finally, funding was raised as a challenge when conducting new research related to health and design (See “Funding” below). Participants associated funders’ lack of interest in part to the public’s lack of awareness and demand regarding buildings and spaces that promote health (see “Public Awareness”).
Measures: Thought leaders were asked about ways in which they or other architects and scientists have measured impacts of intentional spaces on health. They listed a number of physiological measures such as heart rate, cortisol/stress (saliva), medication use, mobile EEG, and eye tracking. Other measures included academic performance, productivity, divergent thinking, problem solving, innovation, social cohesion, perceived productivity, satisfaction, belonging, well-being, pro-sociality, cognitive development, sense of identity, and sense of place. Movement tracking and cognitive development were also discussed. It was unclear how many of these measures are currently in use by the participants or the field at large.
Technology: Related to measures, participants discussed benefits and drawbacks of various technologies used to collect data. They identified movement tracking as particularly helpful given that it is a non-invasive way to observe how people use a space; however, they cautioned that it cannot fully capture or explain how a space affects an individual. For example, one participant argued that efficiency and proximity are often assumed to be obvious goals:
But if the distance [from point A to point B in a building] is longer, and somebody feels better because [that distance now provides a great view or experience], what's the value of that back to performance? or feeling as if you're part of an organization where you want to be there, you want to work there, you want to go there?
Similarly, virtual reality (VR) was mentioned as beneficial because, unlike physical spaces, a researcher can relatively easily change the environment for purposes of experimentation. However, participants argued that ultimately it is still a simulation and thus may not provide an accurate impression of the health effects of a physical environment.
Translating research into practice: Participants emphasized that the successful translation of research into practice will require research to become more accessible. One reason that participants gave for this idea is that architects are typically not scientists (see “Interdisciplinarity”); they thus may not have access to scientific journals, or they may find it difficult to cut through scientific or academic jargon. As one respondent put it, “[T]here was a huge gap between how this information was being understood and read and discussed in academic circles” versus how it was understood, read, and discussed by architects and other practitioners working in communities. This individual asserted that research needed to “be communicated in a way that the industry would understand [and] would see value in it, and take it up.”
Participants also indicated the importance of considering the needs and values of various stakeholders when designing and conducting research, including residents, architects, educators, and others. They traced failures to implement research findings in part to inadequate access to research and limited recognition of its applications across domains: “[A]ll of this research is being done to make a change in the real world. And my concern is that if there is no passion, no motivation to utilize that, then I think these are going to be just some nice papers and interesting studies, not making any change in people's daily lives.”
Theme V: Funding
According to study participants, the current lack of funding for architecture, design, and health initiatives can be traced to limitations of existing funding structures. One participant argued that funding is “an issue because people don't always know where to put people like me [a neuroscientist working in partnership with architects]. And there is no selection committee [at funding organizations] that's going to have the right kind of expertise to evaluate my proposals." Thought leaders asserted that grant review panels lack the interdisciplinary representation needed to adequately understand the complexities of this work. They viewed this as true across funding types and groups—whether related to health, architecture, or design. As a result, participants saw panels as unable to recognize the value of initiatives that bridge disciplines. They suggested that moving forward, review panels should be curated to include reviewers from different fields (e.g., architects, neuroscientists, cognitive scientists, planners, public health experts) who can evaluate both the health and design aspects of proposed work, and assess the value of collaborative initiatives.
Another explanation provided for the lack of funding was that the work is not viewed as “scientific or rigorous enough,” and thus “there is a need for [more] evidence-based research to support the work.” Participants agreed that evidence-based design can contribute to the rigor, validity, and demonstrated impact of the proposed work, which they recognized as necessary for obtaining funder “buy-in.” They also indicated that, because funders are gatekeepers, understanding their perceived barriers could be vital to advancing initiatives in this field: “What would make it easy for you [the funder] to say yes?”
Theme VI: Recommendations
Respondents in each group identified several recommendations to advance intersections of health and the built environment.
Definitions of success: Each focus group offered examples of how they would define “success” in this field, with the most prominent being increased support for “healthy individuals and healthy communities.” They also defined “success” as the existence of more built environments that support human flourishing, and a minimization of “the number of buildings and projects and so on that deplete human flourishing.”
Some participants said they will know the field is successful when there exists an improved, standardized process for designing buildings that reflects the ability to optimize wellness via the built environment. Others hoped to see a future in which a building’s design process was “generative;” in other words, it would be seen not as finished but as an ongoing, dynamic feature of a community—the impacts of which can be continually assessed to inform modifications. Others mentioned that success in this field would have an impact on “schools that educate our children… hospitals or health care facilities that improve the quality of treatment and recovery from disease, people who work in an environment that makes them happy, that makes them comfortable and smarter…cities that are healthier and safer.”
Focus groups also indicated that in a successful field, design teams would be “interdisciplinary” and “include consultants on environment, environmental psychology and neuroaesthetics.” Echoing the “Engagement” theme, participants also wanted to see more inclusion of communities impacted by buildings and their designs. In one respondent’s “romanticized version of the future, we'd have something a lot more equitable… What essentially, I'm talking about...is a handover of control or power in some sense to communities, who can [then] have a bigger influence on the decision making.” Respondents mentioned the ability for design to “bring people together” when “a lot of [current] design just isolates people.” Another added that architecture and design “can bring a sense of optimism and happiness…especially in these stressful, stressful lives that you're having these days, regardless of our location…this sense of happiness is extremely important.”
Training and education: Participants perceived that a major limitation in the work of design for health is that architects are not typically trained for the "human experience," which one respondent defined as "how design will influence the inhabitants of the built environment." They also noted that architects are not necessarily "trained to be interdisciplinary,” but that if they were, they would have “the tools to apply this knowledge [about the health impacts of design] in the way they work, in order to influence their clients and change the profession.” Notably, one individual was critical about a more generalist, interdisciplinary education:
Of course, we like to talk about breaking disciplinary boundaries, creating interdisciplinary, transdisciplinary…and whatnot programs [but] the danger there, of course, is that we will create a dilettante who is curious to talk about all the subjects but is not capable of producing good work in any of these disciplines. This is the danger.
Despite this criticism, other experts agreed that interdisciplinary training supports students' potential for success.
Participants also mentioned the need to incorporate health into design education. This referred not only to curricula and core competencies in schools of architecture, but also K-12 curricula. One participant contended that an emphasis on design and the built environment in K-12 could help “prevent this disciplinary segregation” by “building into young minds” the recognition of design and health as naturally connected.
Respondents additionally discussed the value of including health as a tenet of design excellence; one argued that “if we're looking at elite architecture, we're looking at ‘design excellence.’ We're looking at what is award-winning architecture. [And] I don't think we yet are considering design for health within that.” Another elaborated on this: “The more we can link our work [architecture and design] to basic changes that need to happen in the world we live in,” such as improved health, “the more successful we will be.”
Aspects of design: Participants emphasized the importance of involving multiple stakeholders, including end users, in designs. Viewing design as an ongoing process was also important to participants, one of whom asserted that “ideally, buildings would be tunable to what we need, and there would be a way to adjust and adapt and have them grow as we need them.” They said this will require a “loosening up” of the current conceptualization of buildings “being designed, being constructed, or being finished,” since research-based modifications should be expected once a building is in use. Participants also mentioned the need for design to expand the “boundary conditions” of building projects, given that health or well-being effects are influenced by broader surroundings. For example, the design of a single classroom would need to also consider “the way you got to the building.”
Sustainability and ethics: The issue of sustainability is coded with ethics because it was only discussed in tandem with the ethical responsibility to consider how the realities of climate change should affect building projects. One participant warned there are “serious ethical issues about becoming an architect now,” given the detrimental climate effects of many building projects. Another asked, “What sort of buildings are we going to need in five years, 10 years with a completely different climate?”
Considering ethics beyond sustainability, participants noted that architects can be limited in their ability to attend to health effects, sustainability, or other project impacts due to the nature of the architect-client relationship. One mentioned that architects’ clients are typically also their employers, saying, “the architect just is scared to stand up for anything, even if they believe in it, because their livelihood is really reliant on” the project. As a result, the architect's role tends to mirror the ethics of the person paying them, because “there isn't any mechanism...for architects to call up when, you know, bad decisions might be made.” This respondent wondered if the field of architecture could establish a kind of professional review board to consider ethical issues as they arise on the job, similar to boards that doctors or engineers have.
Issues of ethics were also threaded throughout the “Engagement” theme (above), including equitable community and stakeholder engagement and creating ways for the public (users, residents, etc.) to hold “owners or commissioners” accountable for the health effects of their environments. Ethics were also considered in relation to research regarding health effects: “I was thinking when we were talking now about evidence and impact, you know, what if you had to prove your ability to do no harm? You know, we're talking about how to prove it does good; what if you had to prove that it does no harm?” Finally, one participant stated that working to ethically link the built environment to well-being outcomes presents
The opportunity…to bring back architecture to become an empathy-based profession, which is probably what it should aspire to. And maybe in the past, I would have said that's how it started. But actually, now I think differently. I think the architecture profession became a tool for control for the rich and powerful most of the time.
While increasing studies have illuminated the effects of built environments on health and well-being, the multidisciplinary nature of the field has limited translation, application, and accessibility of research findings. Given these barriers and the emerging nature of the field, it was important to hear directly from international thought leaders who have experience applying health research to architecture, design, and placemaking.
Our initial literature review found many studies that highlight intersections of health and design. Nevertheless, multiple study participants discussed a lack of evidence-based research. This suggests that dissemination and application across disciplines is not yet robust enough to reach even those who are deeply invested in this field, such as the thought leaders in our focus groups. In other words, the siloed nature of this emerging field can be recognized in a lack of shared information and knowledge bases. Participants’ expressed desire for additional research may also indicate a need for studies that can provide models of and indications for varied, specific types of built-environment settings, needs, and potential outcomes.
Study participants generally agreed on current opportunities and promising signs, including: historical shifts (such as the pandemic) that have heightened awareness of the health impacts of buildings; burgeoning interest among younger researchers and practitioners; and increasing consideration of how health research contributes to architecture and design. Throughout the study, an emphasis was placed on public engagement as an essential driver of the demand for buildings and spaces that support health. Participants were clear about existing challenges, including the difficulty of obtaining funding, developing interdisciplinary teams, and conducting rigorous research. They also discussed multiple recommendations, with priorities placed on improved public education and outreach, and opportunities for interdisciplinary work–including frameworks that move teams beyond superficial interaction to ongoing, meaningful collaboration. Participants also prioritized the need for funding structures designed for interdisciplinary projects, inclusion of health as an aspect of practitioner education and design excellence, and increased acknowledgement that buildings’ cost-benefit analyses must include the health of users and the broader community. More generally, participants offered definitions of fieldwide success which, although they did not always illuminate concrete directives, provided an overarching recommendation for where the field should head.
Throughout, several study participants emphasized that any project’s users and local communities should be meaningfully involved in decision-making, building and research processes, and the sharing of related findings. In stressing that research should generate practical change, they focused on equity—arguing that applications of scientific findings and best practices related to health and the built environment must prioritize marginalized and vulnerable populations. Thought leaders also conveyed the importance of considering and addressing climate change, linking the work of intentional spaces with broader environmental health needs.
Trustworthiness in this thematic analysis was supported by an interdisciplinary, interinstitutional team; de-identification of transcripts; iterative discussions and coding rounds with peer agreement; and detailed descriptions of results. In addition, the multidisciplinary nature of curated focus groups helped ensure a range of answers informed by the many disciplines involved in work at intersections of health and the built environment. That said, potential participants were limited by the study’s sampling method; it is possible that contributions by individuals unknown by or unresponsive to the initiative might have altered findings. For example, nearly half of participants (6/13) had expertise in the field of architecture, which may have affected study results.
Regarding future directions, some research concerns may be ameliorated by increased interdisciplinary dialogue regarding study designs and research processes. For example, some study participants appeared to view the required functionality of buildings as existing in opposition to the requirements of research experimentation. Similarly, at least one study participant appeared to associate the need for experimentation in this field with the potential for architectural mistakes. However, the purpose of experimentation is often to determine, within the performance of a needed function, which practices deliver better or worse outcomes. And experimenting toward improved health outcomes would typically involve building sound structures with well-being outcomes in mind, and then testing whether (and to what extent) expected outcomes are delivered. In other words, individuals working in this field need not choose between research and functionality, or between innovation and safety.
Related, study participants focused on quantitative measures when discussing research, apparently due to an impression that these are favored by funders, policymakers, and other decision makers. However, the value of any form of evidence is highly dependent on its end user(s);27 varied forms of knowledge generation and data collection–ranging from digital biomarkers to community storytelling–are likely to have differential value across the many stakeholders and applications involved in this field.
These concerns reflect thought leaders’ interest in innovating, further developing the evidence base, and developing co-created efforts that deliver meaningful outcomes across disciplines, industries, and users. The reservations they expressed suggest that, if research concepts and processes are better shared and understood across interdisciplinary boundaries and experiences, we are likely to see an expansion of professional interest, research designs, and collaborative opportunities in this field.
While the current study illuminates the state of the field as well as actionable recommendations for growth, future research should examine specific built-environment initiatives in this field to better understand the circumstances under which interdisciplinary teams form, who is involved, how they collaborate, the kinds of results they generate, and how these are shared. Mechanisms of support for such endeavors (e.g., funding, education, facilitation, logistics) also suggest important sites of further study. Finally, this study’s themes related to engagement, equity, and ethics indicate the necessity of investigating how and for whom “intentional spaces” are created.
Importantly, this study informed the development of the interdisciplinary “Intentional Spaces Summit,” a highly interactive, collaborative event hosted by the International Arts + Mind Lab at Johns Hopkins School of Medicine. The Summit designed to extend the inquiries and opportunities begun by the present study, and to lay groundwork for further research to inform and improve this area of practice.
This study gathered thought leaders at intersections of health with architecture, design, and placemaking, in order to ascertain their views on the state of the field, current gaps and opportunities, and recommendations. Six themes were identified, with participants emphasizing the need for public and professional awareness, interdisciplinary collaboration, funding, improved research, and equitable application. Discussions illuminated immediate action steps as well as overarching directions for the field. On the whole, findings indicate extensive promise in the field, while identifying several barriers and needs. They affirm that multiple opportunities exist to improve health and well-being outcomes through design, architecture, and the built environment, and that robust interdisciplinary processes could help ensure these opportunities are taken up to further support health and health equity.
None.
This Research Article received no external funding.
Regarding the publication of this article, the authors declare that they have no conflict of interest.
- 1. Dahal S, Swahn MH, Hayat MJ. Association between Neighborhood Conditions and Mental Disorders among Children in the US: Evidence from the National Survey of Children's Health 2011/12. Psychiatry J. 2018;2018:5914315.
- 2. Galea S, Ahern J, Rudenstine S, et al. Urban built environment and depression: a multilevel analysis. J Epidemiol Community Health. 2005;59(10):822-827.
- 3. Hassen N. Leveraging built environment interventions to equitably promote health during and after COVID-19 in Toronto, Canada. Health Promot Int. 2022;37(2):daab128.
- 4. Yin J, Yuan J, Arfaei N, et al. Effects of biophilic indoor environment on stress and anxiety recovery: A between-subjects experiment in virtual reality. Environ Int. 2020;136:105427.
- 5. Maxwell L. School building condition, social climate, student attendance and academic achievement: a mediation model. Journal of Environmental Psychology. 2016;46:206-216.
- 6. World Health Organization Regional Office for Europe. Green and blue spaces and mental health: new evidence and perspectives for action. 2021.
- 7. Lankston L, Cusack P, Fremantle C, et al. Visual art in hospitals: case studies and review of the evidence. J R Soc Med. 2010;103(12):490-499.
- 8. Kondo MC, Fluehr JM, McKeon T, et al. Urban Green Space and Its Impact on Human Health. Int J Environ Res Public Health. 2018;15(3):445.
- 9. Evans GW. The built environment and mental health. J Urban Health. 2003;80(4):536-555.
- 10. Ellard C. Neuroscience, Wellbeing, and Urban Design: Our Universal Attraction to Vitality. Psychological Research on Urban Society. 2020;3(1):6.
- 11. Christian H, Zubrick SR, Foster S, et al. The influence of the neighborhood physical environment on early child health and development: A review and call for research. Health Place. 2015;33:25-36.
- 12. Sarkar C, Gallacher J, Webster C. Urban built environment configuration and psychological distress in older men: results from the Caerphilly study. BMC Public Health. 2013;13:695.
- 13. I’DGO. Why does the outdoor environment matter? Key messages from Inclusive Design for Getting Outdoors. Department of Health, 44(0).
- 14. Van Lier LE, Utter J, Denny S, et al. Home Gardening and the Health and Well-Being of Adolescents. Health Promot Pract. 2017;18(1):34-43.
- 15. Brielmann AA, Buras NH, Salingaros NA, et al. What Happens in Your Brain When You Walk Down the Street? Implications of Architectural Proportions, Biophilia, and Fractal Geometry for Urban Science. Urban Science. 2022;6(3):3.
- 16. Corcoran R, Mansfield R, Giokas T, et al. Places Change Minds: Exploring the Psychology of Urbanicity Using a Brief Contemplation Method. SAGE Open. 2017;7(2).
- 17. Buttazzoni A, Parker A, Minaker L. Investigating the mental health implications of urban environments with neuroscientific methods and mobile technologies: A systematic literature review. Health Place. 2021;70:102597.
- 18. Pykett J, Osborne T, Resch B. From Urban Stress to Neurourbanism: How Should We Research City Well-Being?. Annals of the American Association of Geographers. 2020;110(6):1936-1951.
- 19. Adli M, Berger M, Brakemeier EL, et al. Neurourbanism: towards a new discipline. Lancet Psychiatry. 2017;4(3):183-185.
- 20. Scott S. Learning spaces: Biophilic design in schools. Teacher Magazine. 2020.
- 21. Iyendo TO. Exploring the effect of sound and music on health in hospital settings: A narrative review. Int J Nurs Stud. 2016;63:82-100.
- 22. Franklin N. Biophilic design the key to improving mental health, productivity and stress levels. Workplace Insights. 2018.
- 23. National Organization for Arts in Health. Arts, health, and well-being in America [White paper]. San Diego, CA: Author. 2017.
- 24. MacLeod M. What makes interdisciplinarity difficult? Some consequences of domain specificity in interdisciplinary practice. Synthese. 2018;195:697–720.
- 25. Manning N. Sociology, biology and mechanisms in urban mental health. Social Theory and Health. 2019;17(1):1–22.
- 26. Braun V, Clarke V. Using thematic analysis in psychology. Qualitative Research in Psychology. 2006;3(2):77-101.
- 27. Belfiore E. Is it really about the evidence? Argument, persuasion, and the power of ideas in cultural policy. Cultural Trends. 2021;31(4):293-310.

