The breathing mechanism has existed since our birth and accompanies us throughout life. Breathing is an important function in the regulatory process of numerous body functions, its optimization can bring many health benefits. However, many children are unaware of the mechanisms of breathing, namely abdominal or diaphragmatic breathing, and in addition to this, many breathe normally through their mouths. The present study aimed to verify the influence of a short-term breathing exercise program on children's breathing capacity. Twenty-one children aged between 8 and 10 years were selected, from this selection two groups were formed, the control group (CG) with 10 children and the experimental group (EG) with 11. Through a spirometric test, an assessment of breathing capacity (ABC) was carried out for both groups. The GE participated in a program of breathing exercises (BEP) lasting 15 to 20 minutes for 5 weeks. Then, the ABC was performed again for both groups. The results demonstrate a significant increase in the values (p<0.027) of the forced vital capacity (FVC) of the EG, thus suggesting that the application of a BEP promotes the breathing capacity of school-aged children. Further studies should be performed with larger samples and with a longer protocol.
Keywords: Education, School aged, Children, Breath, Breathing exercises, Spirometry, FVC.
Child development studies increasingly present new observation themes,1-3 which can range from the importance of the socio-affective component and interpersonal relationships with children4 to the importance of structured physical activity5-8 and even highlight the benefits of concentration,9 relaxation and meditation, commonly associated with mindfulness.10 Thus, new fields of investigation appear that contribute to a greater knowledge of the child's evolution process, in harmony with the environment that surrounds him. One of the practices, present in our day-to-day lives and in many areas of research, often overlooked or lessened, is Breathing. The breathing mechanism has existed since our birth and accompanies us throughout life. We understand it commonly by a static and acquired process, however and mainly in the West, we do not always breathe correctly. Many children are not aware of abdominal or diaphragmatic breathing and, in addition to this, they normally breathe through their mouths. Such facts lead to several problems that are not always identified.
We can define breathing as;
- 1. The movement of air or dissolved gases in (inhalation) and out (exhalation) of the lungs
- 2. The physical and chemical processes by which an organism supplies cells and tissues with the oxygen necessary for metabolism and frees them from carbon formed in energy-producing reactions11
This process is considered a key function of the body because it has several functions that contribute in an essential way to self-regulation and homeostasis, such as
- 1. The regulation of the metabolic and chemical functions of the blood, taking oxygen (O2), eliminating carbon dioxide (CO2) and keeping the blood pH at appropriate levels
- 2. The regulation of the autonomic nervous system (ANS)
- 3. Promoting synchronization of the body's oscillatory systems with the breathing rhythms, which optimizes the functions of all systems
- 4. Regulation of the circulatory system, by influencing heart rhythms and blood flow in the body
- 5. Influence on the lymphatic system, contributing to the drainage of toxins through the movements of the breath
- 6. Regulation of psychological states and
- 7. Participation of the breathing muscles in postural and motor control12-15
We understand that breathing is an important function in the regulatory process of numerous body functions, its optimization can bring many health benefits. Studies reveal that the use of breathing, through specific exercises can be beneficial for the prevention of cardiac events,16-18 for the treatment of asthma19-25 of anxiety, stress, post-traumatic stress disorder and depression.26,27 Studies like that of Petrofsky et al.28 demonstrate that daily breathing exercise programs promote improvements in sleep, strength, weight and fat loss and in the increase of oxygen saturation in the blood of young people between 15 and 17 years old. According to the literature review presented by Calmon,29 exercises based on diaphragmatic breathing promote clinical improvements in children in diseases such as asthma and cystic fibrosis. Birkel30 presents a study that demonstrates that the set of breathing techniques improves the vital capacity of the lungs in young students. Also Kupershmidt31 in his study he found an improvement in lung function in individuals who participated in a breathing exercise program for six weeks. This pilot study demonstrated an improvement in the participants' maximum expiratory flow rate and forced expiratory volume. The aim of this study was to verify the influence of a short-term breathing exercise program on children's breathing capacity.
Study participants
The present study was carried out with 21 children, of both sexes, aged between 8 and 10 years old, students in the 3rd year of the 1st cycle of public basic education in the municipality of Matosinhos (Portugal). From these 21 children, two groups were formed: the control group (CG) composed of 10 students and the experimental group (EG) with 11 students. All parents and guardians, as well as the direction of the school group, were informed about the details of the program to be applied (BEP), as well as the procedures for assessing breathing capacity (ABC), before (pre-test) and after (post-test) the application of the program.
Procedures
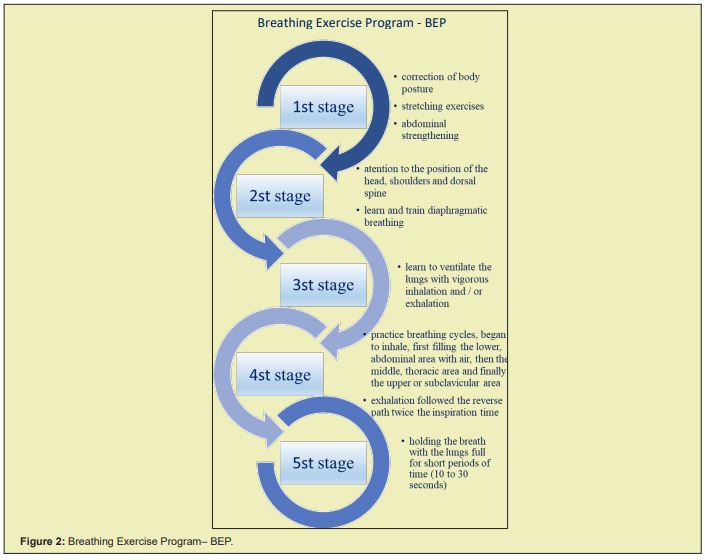
In a first phase, both groups were assessed through a physical examination, where we identified height, weight and sex, and the assessment of breathing capacity (ABC). ABC was performed through a spirometry test with the Air-Smart Spirometer® equipment, validated by Ramos et al.32 In this evaluation we analyzed the forced expiration maneuver to obtain the values of forced vital capacity (FVC); the maximum expiratory volume in the 1st second (FEV1); the peak expiratory flow or maximum expiratory flow (PEF) and the duration. After the first assessment, the GE followed the daily BEP for five weeks. This program was carried out at the beginning of each class with duration of 15 to 20 minutes. The first part of the program focused on the correction of body posture through stretching exercises of the accessory muscles of breathing, stretching of the pectoral and great dorsal muscles, abdominal strengthening in order to favor the diaphragmatic work. The children were also sensitized to a posture correction with attention to the care with the position of the head, shoulders and dorsal spine. The second part consisted of learning and training for diaphragmatic or abdominal breathing. After learning how to use the diaphragm, through the abdominal muscles, the third part of the BEP was carried out, where the children learned to “ventilate” their lungs with vigorous inhalation and/or exhalation. The fourth part of the program consisted of creating breathing cycles where the child began to inhale, first filling the lower, abdominal or diaphragmatic area with air, then the middle, intercostals or thoracic area and finally the upper or sub clavicular area: exhalation followed the reverse path twice the inspiration time. The fifth and last part of the training, after mastering the breathing cycle (fourth part), consisting of holding the breath with the lungs full for short periods of time (10 to 30 seconds). After the BEP was completed, the breathing capacity was reevaluated following the same procedures as the initial ABC. Based on the results of the pre-test and post-test, a comparative and descriptive analysis of them was carried out through the analysis of variance of two criteria (ANOVA) in the program SPSS version 20.
The children who participated in this study were 67% female and 33% male (CG 70% female, 30% male; GE 64% female, 36% male). With regard to age, 90% were 8 years old, 5% 9 years old and 5% 10 years old (GC 82% aged 8, 18% aged 9; GE 82% aged 8, 9% aged 9 and 9% 10 years old). As for the body mass index (BMI), the EG presented an average of 17.24 and the CG, 18.64 (Table 1).
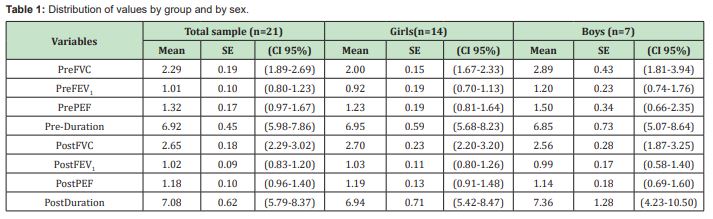
Intra-subject factors: pretest vs. post-test and inter-subject factors: GC vs. GE. Table 1 shows the distribution of values by group and by gender during the pre-test and the post-test. According to the Levene`s test, the groups did not show significant differences with regard to age (p=0.44), sex (p=0.56) and BMI (p=0.44).
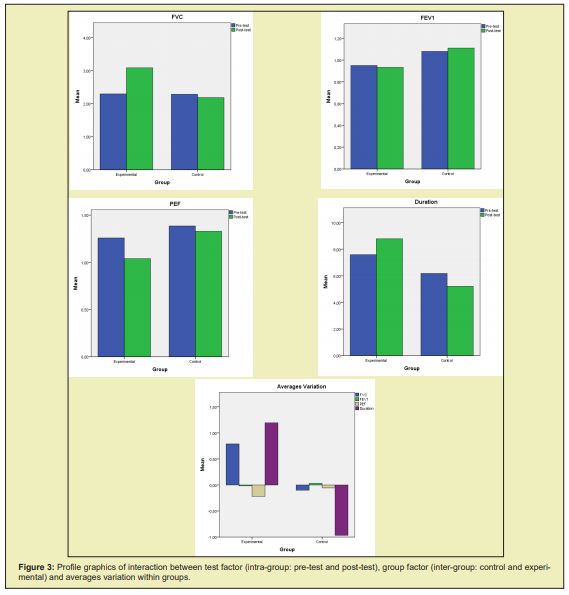
Table 2 Analysis of variables by test and by group. ANOVA multiple comparison test. No significant correlations were found regarding the interaction with the intra-subject factor (Table 2). The results of inter-subject factor, show superior values in the FVC of EG (p<0.027). No significant correlations were found at the remaining results (FEV1, PEF and Duration).
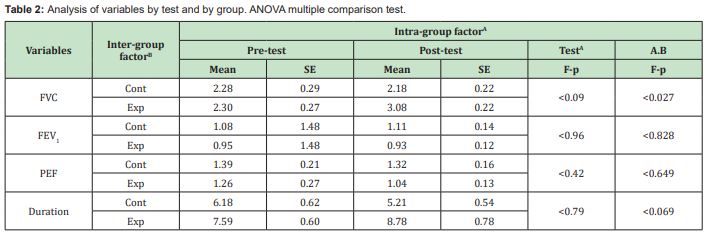
Figure 1. Interaction between the group factor (inter-subject: CG and GE)
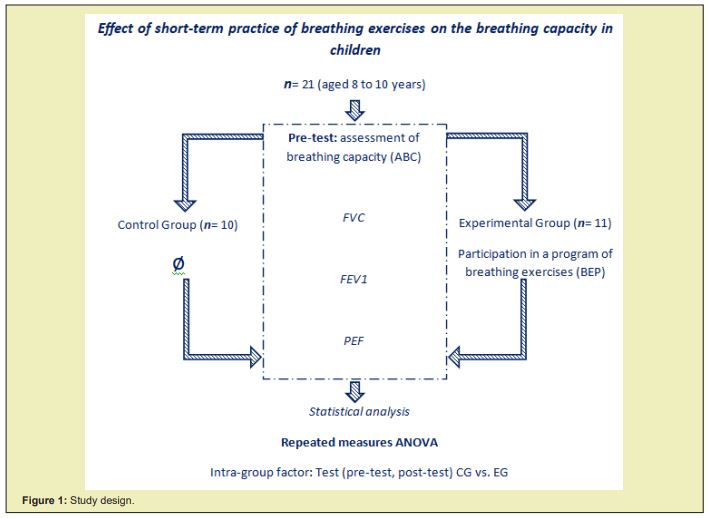
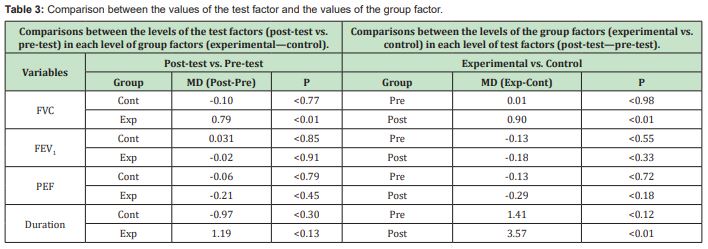
Table 3 shows the variation in the averages of the test results of the two groups. It appears that the variation of the FVC values from the pre-test to the post-test were significant in the EG (p<0.01). No significant correlations were found at the remaining results (FEV1, PEF and Duration).Regarding the variations of the means of the post-test between groups, there are significant changes in FVC (p<0.01) and Duration (p<0.01) in the EG.No significant correlations were found at the remaining results (FEV1 and PEF) (Figures 2&3).
According to the World Health Organization,33 about 235 million people suffer from asthma, most of them children. More and more, studies demonstrate that the use of adequate breathing exercises, have benefits in the recovery of several diseases, both in a clinical approach34-38 as in the improvement of the individual's capacities, in a more holistic approach.39 This study aimed to investigate the influence of a breathing exercise program (BEP) on the breathing capacity of school-aged children. When analyzing the results, there is a significant increase in the forced vital capacity (FVC) in the experimental group (EG) both in relation to the results of the CG (p<0.027) and in relation to the variation between the pre-test and the post-test (p<0.01). Like Lima,40 there was a significant increase in the forced vital capacity of children who were subjected to a PBE, also Banstola,41 Holland et al.,42,43 and Sharifi44 refer to the increase in FVC in individuals who underwent breathing training. Authors such as Vinay,45 Yamaguti46 and Pal47 present significant results in the application of short-term programs or training. Han48 mentions in his studies that a short-term breathing training intervention can lead to an improvement in body posture, which can promote a decrease in heart rate, which in turn can be responsible for improvements in the parasympathetic system (ANS). Petrofsky28 presented positive results in terms of physical and breathing capacity in his study where he verified the influence of a short-term BEP (8 minutes) for six weeks. Also in the duration of ABC, there was an increase in EG compared to CG. Although this result was not significant in relation to the pre-test, it suggests a greater lung capacity in the EG.49-57
As limitations of this study, the small sample size of 21 children stands out. In this study, 49 children were evaluated, however, after the initial and final ABC, only 21 evaluations were validated. In addition to the sample size, the short study time. If BEP had been greater than 5 weeks it could have promoted superior results.
The results obtained in this study suggest that the application of a short-term daily breathing training has positive effects on the breathing capacity (FEV) of school-age children.
The study presented can be a starting point for studies with higher samples and with longer application time of the experimental part. Other variables such as gender and age of participants in future studies could also be assessed.
None.
None.
Author declares that there are no conflicts of interest.
- 1. Rodrigues P, Dias A, Rebolo A, et al. Estudosem Desenvolvimento Motor da Criança. Instituto Piaget. 2018.
- 2. Lopes Vítor P, Gonçalves Celina. Estudosemdesenvolvimento motor da criança VIII. Bragança: InstitutoPolitécnico de Bragança, Escola Superior de Educação; Centro de Investigaçãoem Desporto, Saúde e Desenvolvimento Humano. 2015. ISBN 978‒972‒745‒196‒8.
- 3. Souza JMD, Veríssimo MDLÓR. Desenvolvimentoinfantil: análise de um novo conceito. Revista Latino‒Americana De Enfermagem. 2015;23(6):1097‒1104.
- 4. Gomes RM. Social skills in childhood: identifying to intervene. Interacções. 2016;12(42):70‒95.
- 5. Leite ARDDO. Aimportância da educaçãofísicanasprimeirasidades: a perspetiva dos/as educadores de infância e professores do 1º Ciclo do EnsinoBásico. 2019.
- 6. Zeng N, Ayyub M, Sun H, et al. Effects of physical activity on motor skills and cognitive development in early childhood: a systematic review. BioMed research international. 2017.
- 7. Oliveira FDM. Contribuição da Educação Física para o desenvolvimento motor emcrianças no ambiente escolar. 2017.
- 8. Costa HJT, Barcala Furelos R, Abelairas Gomez C, et al. The influence of a structured physical education plan on preschool children's psychomotor development profiles. Australasian Journal of Early Childhood. 2015;40(2):68‒77.
- 9. Somerton Burkhardt HL. Creating A Normalized Montessori Classroom. 2015.
- 10. Champeaux Cunin M, Butet D. The Magic of Meditation: Stories and Practices to Develop Gratitude and Empathy with Your Child. Shambhala Publications. 2018.
- 11. WebMD COPD: Exercise and Breathing. WebMD Medical. 2020.
- 12. Cruz MZ. Breathing as a tool for psychophysiological self-regulation in preschool children: a study based on heart rate variability. Tese de doutoramento. Universidade Estadual Paulista "Júlio de Mesquita Filho", Faculdade de Medicina; Disponívelem: 2016.
- 13. Guyton AC, Hall JE, Zocchi L, et al. Fisiologiamédica (Vol. 11). Madrid: Elsevier; 2006.
- 14. Courtney R. The functions of breathing and its dysfunctions and their relationship to breathing therapy. International Journal of Osteopathic Medicine. 2009;12(3):78‒85.
- 15. Jerath R, Edry JW, Barnes VA, et al. Physiology of long pranayamic breathing: neural respiratory elements may provide a mechanism that explains how slow deep breathing shifts the autonomic nervous system. Medical hypotheses. 2006;67(3):566‒571.
- 16. Yesmin J, Begum N, Ferdousi S. Effect on Time Domain parameters of HRV after slow breathing Exercise in Type 2 Diabetes Mellitus. Journal of Bangladesh Society of Physiologist. 2017;12(1):15‒20.
- 17. Reis JRG, Nascimento LCG, Ramos JM, et al. Programa de exercíciosrespiratórios com sessões de curtaduração e osefeitosnamecânicaventilatória de crianças com asma. Revista Digital. 2015;20(211):1‒9.
- 18. David S Shannahoff Khalsa, B Bo Sramek, Matthew B Kennel, et al. Hemodynamic observations on a yogic breathing technique claimed to help eliminate and prevent heart attacks: a pilot study. Journal of Alternative and Complementary Medicine. 2004;10:757‒766.
- 19. Dressendorfer R, Matlick D, Council RO, et al. Asthma and Exercise. Clinical Review. 2019.
- 20. Marilyn Karam, Bani P Kaur, Alan P Baptist. A modified breathing exercise program for asthma is easy to perform and effective. Journal of Asthma. 2017;54(2):217‒222.
- 21. Cowie R, Underwood MF, Reader PG. A randomized controlled trial of the Buteyko technique as an adjunct to conventional management of asthma. Respiratory Medicine. 2008;102:726‒732.
- 22. Mchugh P. Buteyko breathing technique for asthma: an effective intervention. New Zealand Medical Journal. 2003;116:U710.
- 23. Slader C, Reddel HK, L M Spencer, et al. Double blind randomized controlled trial of two different breathing techniques in the management of asthma. Thorax. 2006;61:651‒656.
- 24. A J Opat, Cohen MM, M J Bailey. A clinical trial of the Buteyko breathing technique in asthma as taught by a video. Journal of Asthma. 2000;37:557‒564.
- 25. Bowler SD, Green A, Mitchell A. Buteyko breathing technique in asthma: ablinded randomized controlled trial. Medical Journal of Australia. 1998;169:575‒578.
- 26. Mohamed SA. The effects of positioning and pursed‒lip breathing exercise on dyspnea and anxiety status in patients with chronic obstructive pulmonary disease. Journal of Nursing Education and Practice. 2019:9(6).
- 27. Brown RP, Gerbarg PL. SudarshanKriya yogic breathing in the treatment of stress, anxiety, and depression. Part I– neurophysiological model. Journal of Alternative and Complementary Medicine. 2005;11:189‒201.
- 28. Petrofsky J, Laymon MS, Khowailed IA, et al. The effect of an 8‒minute yoga breathing program on fitness, weight loss and breathing capacity. Journal of Applied Medical Sciences. 2016;5(4):57‒80.
- 29. Calmon CMS, Góes DL, de Oliveira Bermudez DG, et al. Diaphragmatic Breathing Exercise in Children. Manual Therapy, Posturology& Rehabilitation Journal. 2017;14.
- 30. Birkel DA, Edgren L. Hatha yoga: improved vital capacity of college students. Alternative therapies in health and medicine. 2000;6(6):55.
- 31. Kupershmidt S, Barnable T. Definition of a Yoga Breathing (Pranayama) Protocol That Improves Lung Function. Holistic nursing practice. 2019;33(4):197‒203.
- 32. Cristina Ramos Hernández, Marta Núñez Fernández, Abel Pallares Sanmartín, et al. Validation of the portable Air Smart Spirometer. PloS one. 2018;13(2):e0192789.
- 33. Organização Mundial da Saúde. Chronic respiratory diseases (OMS/WHO). 2020.
- 34. Manandhar S, Pramanik T. Immediate Effect of Slow Deep Breathing Exercise on Blood Pressure and Reaction Time. Mymensingh medical journal: MMJ. 2019;28:925‒929.
- 35. Gamboa A, Smith EC, Paranjape S, et al. Abstract P3057: Slow Breathing Training Reduces Blood Pressure in Healthy Normotensive Subjects. Hypertension. 2019;74(Suppl_1):AP3057‒AP3057.
- 36. Harvard Medical School. Relaxation techniques: Breath control helps quell errant stress response. Harvard Health Publishing. 2018.
- 37. Vieira FM, de Souza Fernandes F, Reichow JRC, et al. O Trabalho Respiratóriocomo Ferramenta Psicoterapêutica: Uma Revisãoembasadana Psicologia Corporal. Revista Latino‒Americana De Psicologia Corpora. 2018;7(1):83‒107.
- 38. Hosking S. The effect of osteopathic manipulative techniques on diaphragm movement and respiratory function in asymptomatic subjects. (Unpublished document submitted in partial fulfilment of the requirements for the degree of Master of Osteopathy). New Zealand: Unitec Institute of Technology, Auckland; 2009.
- 39. Marques Patrícia de Souza, Fagali, Eloisa Quadros. The influence of breathing on the learning process. Construçãopsicopedagógica. 2018;26(27):37‒52.
- 40. Lima M. Efeito do treino dos músculosinspiratóriosnafunçãopulmonaremnadadores de competição. 2018.
- 41. Banstola D. Effect of yoga breathing exercises on ventilatory function. Journal of Gandaki Medical College‒Nepal. 2016;9(2):17‒22.
- 42. Holland AE, Hill CJ, Jones AY, et al. Breathing exercises for chronic obstructive pulmonary disease. Cochrane Database of Systematic Reviews. 2012;10:CD008250.
- 43. Holland AE, Alison JA, Harvey A, et al. Respiratory diseases. Cardiorespiratory Physiotherapy: Adults and Pediatrics E‒Book: formerly Physiotherapy for Respiratory and Cardiac Problems. 2016.
- 44. Sharifi G, Babai Mazreno A, Salmani I, et al. Effects of a Period of Selected Activity on Lung Capacities in Children 5‒10 Years with Asthma Caused by Exercise. International Journal of Pediatrics. 2014;2:(3.3):11‒17.
- 45. Vinay AV, Venkatesh D, Ambarish V. Impact of Short‒Term Practice of Yoga on Forced Vital Capacity, Forced Expiratory Volume in 1st Second and Peak Expiratory Flow Rate in Healthy Adults. Annals of Health and Health Sciences. 2017;4(2):62‒66.
- 46. Yamaguti WP, Claudino RC, Neto AP, et al. Diaphragmatic breathing training program improves abdominal motion during natural breathing in patients with chronic obstructive pulmonary disease: a randomized controlled trial. Archives of physical medicine and rehabilitation. 2012;93(4):571‒577.
- 47. Pal Gopal, Subramaniyam, Madanmohan. Effect of short‒term practice of breathing exercises on autonomic functions in normal human volunteers. The Indian journal of medical research. 2004;120:115‒121.
- 48. Han J, Chae Y, Lee NK. The immediate effect of incorporating short‒term slow abdominal respiration into an exercise program on balance and the autonomic nervous system. Physical Therapy Rehabilitation Science. 2019;8(4):225‒233.
- 49. Bortholoto Sandra. Yoga at School-Body-Mind Education for Parents and Educators. São Paulo: Ground; 2013.
- 50. Flak M, Coulon J. Yoga in Education-Integrating Body and Mind in the Classroom. Florianópolis: Editora Comunidade do Saber; 2007.
- 51. Inês Margarete Balthazar, Neuzeli Mariano, Telma Suely Bezerra do Nascimento e Luciana do Nascimento Villena. Breathing And Learning: What Do Teachers Know About The Subject? Proceedings III CONEDU. 2016.
- 52. Lopes da Silva I, Marques L, Mata L, et al. Orientações Curriculares para a EducaçãoPré‒Escolar. Lisboa: ME/DGE; 2016a.
- 53. Lopes da Silva I, Marques L, Mata L, et al. Orientações Curriculares para a EducaçãoPré‒Escolar do passadoaopresente. desafios para o futuro. Cadernos de Educação de Infância. 2016b. p. 4‒14.
- 54. Lopes da Silva I, Marques L, Mata L, et al. Revisão das Orientações Curriculares para a EducaçãoPré‒Escolar, em Portugal. In: FI Ferreira, editors. Atas do II Seminário Luso Brasileiro de Educação de Infância. 2016c. p. 19‒31.
- 55. Sato DL. Yoga naescola. Universidade de Taubaté: São Paulo, Brasil; 2019.
- 56. Sousa F. The Curriculum For Preschool Education Between The Specific And The Common: The Case Of OCEPE. Revista de Estudos Curriculares. 2018;9:24‒44.

